News
Pharmacy reform could save more than $800m annually
Allowing patients two months’ supply of some medications would halve dispensing fees, the RACGP has said.
 The RACGP has said allowing 60-day dispensing for some medications would save hundreds of millions of dollars each year.
The RACGP has said allowing 60-day dispensing for some medications would save hundreds of millions of dollars each year.
In 2018, the Pharmacy Benefits Advisory Committee (PBAC) recommended increasing the maximum dispensed quantities of 143 common medications from one to two months’ supply.
But despite widespread support from doctors and other medical groups, the then Federal Government bowed to Pharmacy Guild pressure and backed away from plans to institute the reform.
Less than three years later, in 2021–22, pharmacy dispensing fees cost taxpayers $1.67 billion – a figure the RACGP says could be halved should the current Government act on the PBAC’s recommendation.
The measure is one of a number of proposed reforms the college has put forward ahead of the May Federal Budget aimed at making medicines cheaper and easier to access.
RACGP President Dr Nicole Higgins said such reforms would not only ease cost of living pressures for Australians but also reduce the administration for scripts, allowing GPs to have more time with patients.
‘We have a cost-of-living crisis and a health system crisis on our hands, and people across Australia are feeling the crunch and struggling to access or afford the healthcare and medicines they need,’ she said.
‘[Allowing] patients to get a larger supply of medicines in one go by increasing the supply interval for certain medicines … will save the Government money on dispensing fees, which could in turn be used to further subsidise patient care.
‘These reforms are an easy way to help those most in need, including people who are older and those with chronic conditions who often need multiple medicines.
‘It will save money for individual patients, as well as significant savings for the overall health budget and taxpayers.’
In 2019, when the Australian Government last considered introducing 60-day dispensing, the Pharmacy Guild opposed the move on the grounds that it would have ‘a devastating impact on the viability of community pharmacy businesses’ and halve the profits for some pharmacies.
More recently, a Guild spokesperson told Nine Newspapers that the pharmacy owners’ lobby group remains opposed to the move, but this time cited safety concerns, rather than profits.
‘The current system of generally providing one month’s supply of a medicine strikes a practical balance between patient convenience and minimising the availability of medicines in a patient’s home, and hence the community,’ he said.
‘When a patient returns to their community pharmacy for a repeat supply of a prescription medicine, pharmacists have the opportunity to access patient compliance with the prescribed medicine, and can intervene if confusion or adverse reactions to medicines are identified.’
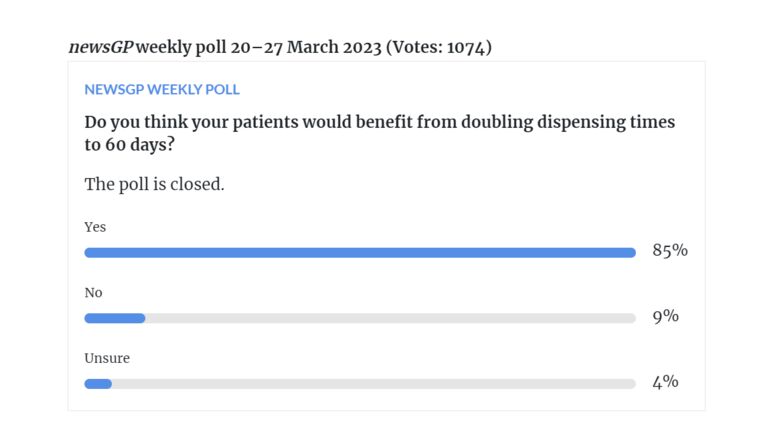
However, a newsGP poll ran last week suggests that the vast majority of GPs do not hold these concerns, with 85% of respondents stating that their patients would benefit from increasing the amount of supply for appropriate medications.
Federal Health and Aged Care Minister Mark Butler appeared at the Australian Professional Pharmacy Conference over the weekend but would not be drawn on whether the Government is considering instituting in the upcoming Budget, stating that the speculation would become ‘clear’ in May.
In addition to enacting the PBAC’s supply recommendation, the college has also proposed that Government:
- extend the length of prescriptions to increase from the current six-month limit to 15 months for suitable patients
- investigate the benefits of removing the $1 discount rule, which caps discounts on medicines
- overhaul Australia’s anti-competitive pharmacy ownership and location laws, which inflate costs for patients
- make prescribing faster and easier for GPs so they have more time for patient care by streamlining the Pharmaceutical Benefits Schedule (PBS) prescribing system, which it says is unnecessarily complex.
When announcing the proposed reforms, Dr Higgins said the health system crisis must be tackled from all sides, and that making medicines cheaper and easier to access would save patients time and money, reduce the overall healthcare budget, and free up GPs.
‘Australia needs to seriously explore alternative models to lower the cost of medicines and increase access and choice for people across Australia,’ she said.
‘Other models such as supermarket pharmacies, online pharmacies and automated dispensing machines are used widely in other western countries like the US and UK, and could make a real difference here, particularly in rural communities.
‘Everyone deserves access to affordable and high-quality primary care and medicines, no matter their postcode or income. But too many people are missing out, which is causing more people to go to hospital, and more pressure on our overstretched emergency care system.
‘The Government should … use the Budget to act on these reforms to make medicines cheaper and easier to access. It is an easy way to help Australians battling rising costs at a time when they really need it.’
Log in below to join the conversation.
dispensing fees Federal Budget pharmacy reform
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?