News
Rapid move to telehealth can be complex – but essential for safety
Telehealth is now available to all Australians, but how do you quickly shift away from face-to-face consultations?
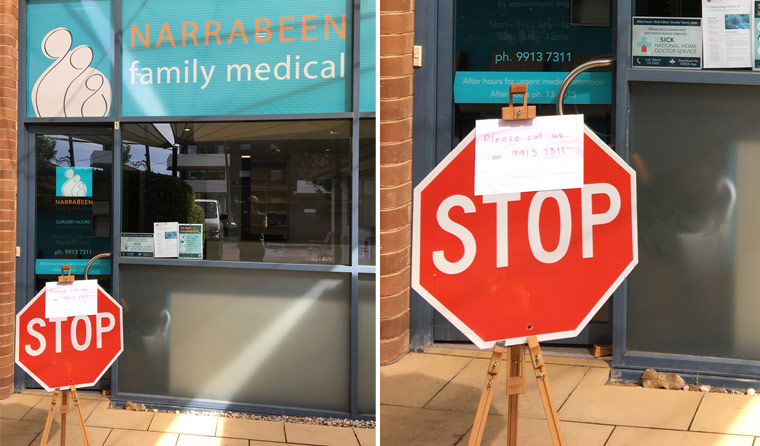 A patient passing a prominent sign stating that anyone with respiratory symptoms should not enter was a tipping point for Narrabeen Family Medical.
A patient passing a prominent sign stating that anyone with respiratory symptoms should not enter was a tipping point for Narrabeen Family Medical.
The tipping point came two weeks ago.
A parent brought a child in to see their GP on Sydney’s northern beaches. To get into the clinic, the patient had gone past a prominent sign stating that anyone with respiratory symptoms should not enter.
Now that she was in the consultation room, the parent revealed her child had symptoms of an upper respiratory tract condition.
That was the last thing her GP wanted to hear.
‘It was like, “Oh my god”,’ practice owner Dr Nick Bernard said.
What Dr Bernard took from the incident was simple: You cannot rely on patients to self-screen.
Dr Bernard immediately began to plan a rapid-fire move to telehealth, aided by the GPs, nurses and staff of Narrabeen Family Medical.
‘As an employer I have a responsibility to my staff and we weren’t able to put in adequate protection, especially for the reception staff. We had limited quantity of hand sanitiser and masks,’ he said.
At that time, the Government had not yet expanded telehealth Medicare Benefits Schedule (MBS) items to all patients.
But Dr Bernard told newsGP that the protection of his staff was paramount.
Practices around Australia have struggled to source enough personal protective equipment (PPE) to guarantee the safety of frontline GPs, practice nurses and reception staff.
‘We didn’t have PPE, just basic masks, rubber gloves and eye protection I bought myself,’ he said.
‘We were seeing minor respiratory infections that could have been dealt with over the phone.
‘I was getting anxious myself. I’m 58; if I get COVID-19 it could be really life-threatening.’
So Dr Bernard closed the practice doors to everyone except for patients who required a face-to-face consultation, for issues such as skin rashes.
That meant no danger of spreading the virus in crowded waiting rooms, significantly reducing danger to frontline staff, and the conservation of scarce PPE stocks.
In-practice patients are now screened at the door and asked if they have a respiratory infection, if they have recently travelled overseas, or if they have had close contact with a person with coronavirus.
Staff members wearing gloves, masks and protective eyewear take their temperatures at the door.
Patients are then seen in a room where everything but the chairs has been removed, to make cleaning easier.
For children’s immunisations, Dr Bernard has brought in a 30-minute appointment minimum to avoid a backlog of patients, and to minimise face-to-face time. Patients are also screened for respiratory illness, travel history and potential coronavirus contact.
For all other patients, it is telephone or video calls only.
‘It’s better now that we’ve moved to telehealth. I still wouldn’t say we’re in a relaxed atmosphere, but people felt better once the systems were in place,’ Dr Bernard said.
As many practices are finding, changing the way medicine is traditionally delivered can come with teething problems.
‘It takes a while to get use to this,’ Dr Bernard said. ‘You have to practice it. Having a two-week lead time has allowed us to get the systems in place.’
For GPs looking to move across to telehealth now that the Government has made it available to all Australians, Dr Bernard has advice: do it today.
‘It takes a little while to build up the systems. We have eight consultation rooms, so this really grinds the gears at first,’ he said.
Unexpected problems arise, such as high numbers of patients arriving to pick up scripts, specialist referrals or medical certificates.
‘We found we had crowds at the front door. So it’s taken us a little while to develop systems where we don’t require patient pickup,’ Dr Bernard said.
And as Australia’s systems groan under the strain of a nationwide shift to online or telephone services, even the workarounds can require workarounds.
Because the NBN does not deal well with faxes, for example, efforts to fax scripts to pharmacies failed.
‘Now we’re emailing scans of the script to the pharmacy and mailing the physical script at the end of the week,’ Dr Bernard explained. ‘We worked out a way of putting our signatures into email so we can email signed medical certificates.’
The sudden shift to telehealth also ran into the issue of a shortage of telephone lines. In the interim, GPs have been using their mobiles to call patients directly.
Dr Bernard even dug up old mobile phones with different sim cards in an attempt to deal with the fact that mobile networks are often congested.
‘We are finding a variety of workarounds,’ he said.
‘It’s been a system of introducing something, running into a problem and finding a workaround.
‘We’re constantly working through problems.’
But although the path to telehealth might be frustrating at times, Dr Bernard believes it is still far better than potentially being exposed to the coronavirus.
The RACGP has more information on coronavirus available on its website.
Log in below to join the conversation.
coronavirus COVID-19 telehealth
newsGP weekly poll
As a GP, do you use any resources or visit a healthcare professional to support your own mental health and wellbeing?