News
Should bulk-billing rates be used as a measure of healthcare success?
While ‘more Australians than ever’ are accessing healthcare at no cost to themselves, GPs argue record bulk-billing rates ignore the threat posed by burnout and ever-increasing business costs.
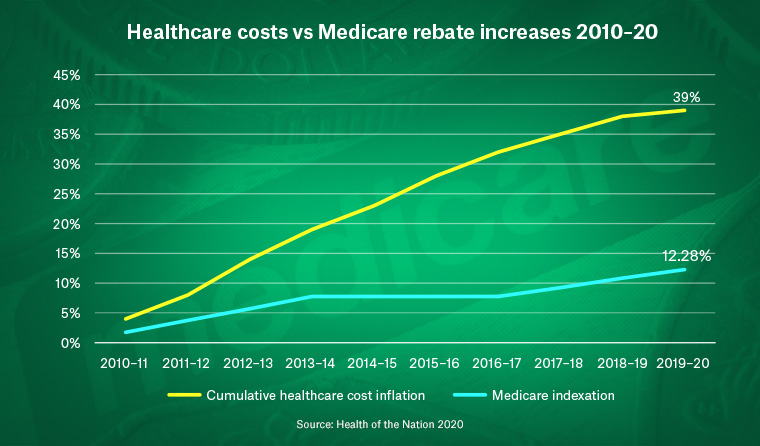 Healthcare cost increases have outpaced Medicare rebate indexation.
Healthcare cost increases have outpaced Medicare rebate indexation.
According to Federal Health Minister Greg Hunt, ‘more Australians than ever’ are getting the medical care they need at no cost to themselves due to ‘record’ high GP bulk-billing rates.
‘Almost nine out of 10 visits to the GP in the nine months to March 2021 [were] provided with no out-of-pocket cost to the patient,’ Minister Hunt said on Sunday. ‘Our government’s commitment to Medicare and bulk billing remains rock solid.
‘These figures show that we are supporting the health and wellbeing of Australians more than ever before.’
However, following the announcement, a host of GPs took to social media to challenge Minister Hunt’s claims and the purported benefits for patients, while also calling for more Federal Government support for general practice, especially in the context of the ongoing COVID-19 pandemic.
From July 2020 to March 2021, bulk billing service rates reached an all-time high of 88.7% for the period, up 6.7% on the same period in 2012–13.
But temporary telehealth items represented 24.8% of all GP consultations during the captured period, around 99% of which were bulk-billed by GPs in 2019–20.
RACGP President Dr Karen Price also told newsGP another way in which the statistics fail to tell the full story is that they only represent the number of services that are bulk billed, not the number of patients who have incurred no out-of-pocket costs.
‘The real figure is probably as low as two-thirds of patients,’ she said. ‘Moreover, what these numbers don’t reflect is the ever-widening gap between Medicare patient rebates, which were stagnant for a number of years, and healthcare inflation.
‘We don’t want to see patients suffer government gaps on their public Medicare insurance. Clearly during the pandemic, our hardworking GPs have been assisting those Australians who have been doing it tough, as well as continuing to cover the costs of rising practice overheads.
‘General practice is the most efficient element of the healthcare system and performs an invaluable service to the community, yet many clinics are struggling to stay afloat due to a lack of investment in primary care and the ongoing effects of the Medicare freeze.’
Prominent Queensland GP and practice owner Dr Maria Boulton, who is also member of the RACGP Expert Committee – Funding and Health System Reform (REC–FHSR), was one of the GPs who commented on Minister Hunt’s Facebook post.
She questioned why funding for primary care is lower in Australia than in other countries, and wrote that quality healthcare is measured by outcomes, not costs.
‘GPs cannot continue to subsidise medical care for Australians. We have expenses – rent, equipment, staff, insurances, electricity, phone, clinical software, telehealth equipment, vaccine fridges, vaccine fridge batteries, etc that need paying,’ she posted.
‘These expenses are charged at 2021 values, not 1980s values like the Medicare rebates.
‘The Medicare rebates as they stand have not caught up with the cost of living. For the sake of our patients listen to what GPs are saying in these comments. Patients deserve more than the rebates cover.
‘GPs need more time to spend with their patients. Especially now that many of our patients are presenting with mental health issues due to the pandemic. GPs continue to do the heavy lifting, it is time for the Government to listen and help GPs as they continue to help patients.’
Another factor creating a ‘major case’ for funding reform and the need to reinvest in primary care, Dr Price says, is the changing needs of a future-proofed workforce.
‘What is worrying, and has been for some time, is the number of young graduates seeking a general practice career,’ she said.
‘Currently, the number of new graduates entering general practice from university sits at around 16%, whereas the number of new graduates entering GP training needs to reach 50% if we are to have an efficient health system.
‘Given the new graduates are often heavily laden with HECS debts and are older than they used to be, some courageous and far-sighted policy is needed.’
Dr Price said the college has been working collaboratively with the Government on improving primary care and will continue to do so by offering strategies geared towards the ‘quadruple aim’ of health system reform.
‘The quadruple aim includes population health outcomes, patient experience of receiving health care, efficiency, and the wellbeing of physicians delivering healthcare,’ she said.
‘Without any of these four components, healthcare service delivery is suboptimal.
‘Bulk-billing rates are not at all a descriptor of a health system, but one solitary marker of the responsiveness of GPs to their communities and the pandemic.’
According to the RACGP, new ways of reforming the healthcare system, such as introducing voluntary patient enrolment, are needed because the current system does not account for the increasingly complex patients being seen in general practice.
Dr Price believes the success of telehealth is an important innovation that the Government can ‘rightly claim credit for’ and for which patients have been helped through an international pandemic.
But she said health officials needs to be mindful that the continued success of a complex system is never one factor.
‘The current fee-for-service system is weighted in favour of high-volume, low-value care and is not sustainable,’ she said.
‘When did the bulk-billing rate become the measuring stick for optimal health and wellbeing?
‘We must invest heavily in preventive health and primary care before it’s too late. Burnout is being exacerbated and if the status quo continues a whole host of amazing GPs will soon be lost to the profession due to stress and exhaustion.
‘The economics of an unsupported health system and its clinicians are far more costly to patients and to taxpayers. I look forward to continued investment and reform where it matters most.’
Log in below to join the conversation.
advocacy bulk billing complex care Medicare telehealth
newsGP weekly poll
As a GP, do you use any resources or visit a healthcare professional to support your own mental health and wellbeing?