News
Should GPs have to write referrals for cosmetic surgery?
The new requirement is part of a host of reforms aimed at cleaning up the industry, but there is disagreement over its appropriateness.
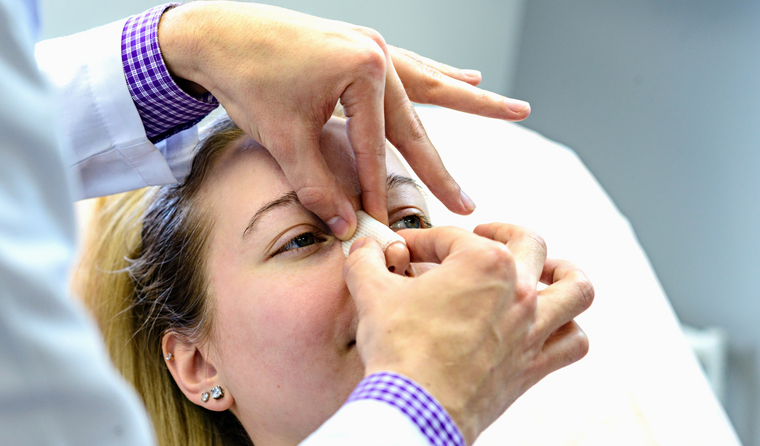 Patients seeking cosmetic surgery will need to have at least two pre-operative consultations as of 1 July.
Patients seeking cosmetic surgery will need to have at least two pre-operative consultations as of 1 July.
AHPRA’s new Accreditation standards for cosmetic surgery endorsement have been released, the latest in a series of reforms aimed at Australia’s ‘cosmetic cowboys’.
Among the Medical Board’s new guidelines is the need for a referral from a GP to their cosmetic surgeon, a requirement welcomed by Dr Ronald Feiner, a former GP who now works exclusively as a cosmetic physician.
‘People will need to see an independent GP, unrelated to the cosmetic surgeon for a referral,’ he told newsGP.
‘There is nothing wrong with that, it’s another layer of safety. GPs have a holistic look at everything that goes on with a patient and this can add to the information load.
‘I don’t think it’s a bad thing and I don’t think many cosmetic surgeons will object to that.’
Dr Feiner says he understands that GPs might not be overly familiar with certain cosmetic procedures, but believes this is no different to other complex conditions that patients get referred for.
‘I know they [GPs] already have a high workload, but overall my gut feeling is that it’s helpful and goes towards patient safety,’ he said.
Dr Feiner also says patients will not need to see a GP if they are considering injectables such a Botox or fillers and other nonsurgical procedures.
However, while there was widespread support for changes aimed at protecting patients from exposure to inappropriate and dangerous practice, not everyone is in favour of how the new reforms have been designed.
Dr Tim Ross, a digital health consultant and Melbourne GP, is one who does not support the requirement for a GP referral.
‘This is a step change, for the worse, in managing healthcare,’ he told newsGP.
‘Previously, no patient needed a referral to see anyone. A referral was a financial control whereby GPs were entrusted to judge the need for other, more expensive specialist care and enable a Medicare rebate to the patient at the referred service.’
Dr Ross says the upcoming change will convert the referral from a financial gatekeeper to a quality gatekeeper and also relies on the GP knowing the competence of the cosmetic surgeon.
‘This is not the job of a GP,’ he said.
‘These are not medical procedures, these are not medical care. There will be huge conflict at the GP surgery as there may be differences in opinion on the need for any cosmetic procedure, yet patients will be requesting referrals as it is the only way they can have their preferred procedure.
‘These are not “medical” needs by definition and should not need to involve the GP, other than as a trusted advisor where a treating relationship exists.’
And while the reforms have been enacted following widespread media coverage regarding harms to patients, Dr Ross says the regulation of cosmetic surgery is being imposed at the wrong end.
‘GPs should not be the arbiters of who does cosmetic surgery,’ he said.
‘Those procedures should be regulated [and] approved by the relevant learned craft, RACS [Royal Australasian College of Surgeons] or similar.
‘There are strict provisions on who is a GP, who is a surgeon, who is a physician. It should be the same for people practising cosmetic surgery, not some bureaucratic referral system.’
Dr Ross’ position appears to be at odds with the RACGP, which last year voiced support for mandatory consultation with a GP or other appropriately trained health professional before a significant cosmetic procedure.
‘A GP would be able to assess the patient for appropriateness of the procedure, and to screen for underlying physical and mental health issues that may need to be considered,’ former President Adjunct Professor Karen Price told newsGP during the consultation phase.
‘GPs should also have access to resources to support patients in these situations, including questions to ask a provider before a procedure, and advice on a cooling off period before committing to surgery.’
She also said pre-surgery consultations with a GP would go a long way towards improving informed decision making.
‘It’s important to note that in many instances GPs don’t have the opportunity to have a conversation with people considering cosmetic medical or surgical procedures, because consumers often bypass their usual GP and go directly to cosmetic practitioners,’ Professor Price said.
‘Making changes here to ensure consumers do consult with their GP, or an appropriately trained health professional, could make a real difference.’
Other changes to the cosmetic surgery guidelines, which take effect 1 July, include that:
- the medical practitioner who will perform the surgery must assess the patient with a validated screening tool for underlying psychological conditions such as body dysmorphic disorder
- a patient seeking cosmetic surgery must have at least two pre-operative consultations
- there must be a cooling-off period of at least seven days after the patient has had two consultations and given informed consent (signed consent forms), before the surgery can be booked or a deposit paid.
Log in below to join the conversation.
AHPRA cosmetic cowboys cosmetic surgery
newsGP weekly poll
As a GP, do you use any resources or visit a healthcare professional to support your own mental health and wellbeing?