News
Strengthening Medicare report recommends funding longer consultations
Greater investment to support multidisciplinary teams in general practice has also been proposed, but increased Medicare rebates are not mentioned.
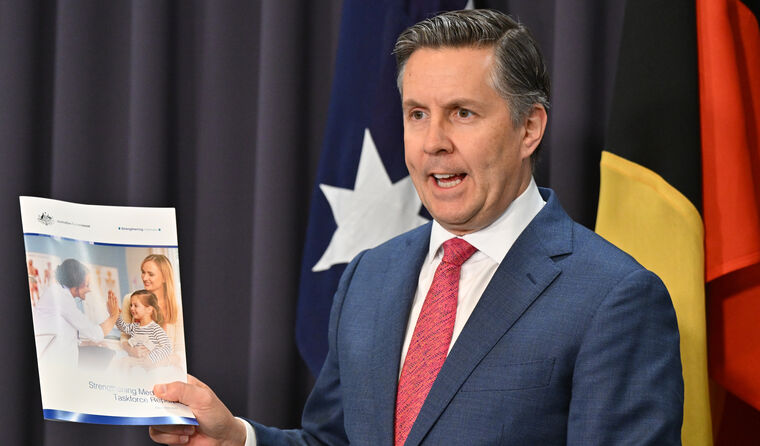 Federal Health and Aged Care Minister Mark Butler at a press conference launching the Strengthening Medicare Taskforce report. (Image: AAP)
Federal Health and Aged Care Minister Mark Butler at a press conference launching the Strengthening Medicare Taskforce report. (Image: AAP)
The RACGP has cautiously welcomed many of the long-term reforms contained in the Strengthening Medicare Taskforce report, which was publicly released after being presented to state and territory leaders at National Cabinet earlier in the day.
The report, which took more than six months to develop, lays out significant reforms to modernise Medicare and bolster general practice, as well as provide high-level guidance to the Federal Government on where it should invest the $750 million it pledged ahead of last year’s election.
Following today’s meeting, Prime Minister Anthony Albanese told reporters that health reform is a ‘first priority issue’ for National Cabinet, and that better integration will be a major focus of the planned changes.
‘The key, going forward, is to better integrate the systems,’ he said. ‘We know that the earlier the care is provided, the cheaper that care will be as well.
‘That is a common position which we have, and we’ll be prioritising that throughout 2023.’
Specific Taskforce recommendations welcomed by the RACGP include:
- funding for longer consultations to reflect the fact that chronic and complex care requires more time than is funded for in a standard consultation
- increasing investment to support multidisciplinary teams in general practice that are responsive to local needs – as long as patients are accessing centrally coordinated care via their general practice
- ‘blended funding models’ integrated with fee-for-service, including incentives to promote better care for people who need it most
- introducing a streamlined and straightforward voluntary patient registration scheme, which enables patients to sign up to a practice that receives extra funding to coordinate care
- better use of data and digital technology to share critical patient information and support superior patient healthcare
- investing in Aboriginal Community Controlled Health Organisations to commission primary care services, building on their expertise and exploring new funding models that are locally relevant for rural and remote practice
- investing in primary care research.
Speaking after its release, RACGP President Dr Nicole Higgins said the report contains many promising elements, but that more action is needed to secure the future viability of general practice care.
‘The RACGP is pleased to have participated in the Taskforce and we are committed to working alongside government to implement reform,’ she said.
‘It is very positive that health reform is, as the Prime Minister said today, a first priority issue for 2023 and to see the states and territories come to the table with the Federal Government to discuss these vital issues.
‘We welcome many aspects of the report but there is a high level of ambiguity, and the devil will be in the detail on many of the recommendations.’
Dr Higgins also said reform without proper investment is ‘hollow’, and that short-term action is needed to ‘stem the bleeding’.
‘GPs and practice teams have experienced many years of neglect and underfunding that has left general practice care in urgent need of an investment boost,’ she said.
‘General practice is the answer to relieving pressure on the entire healthcare system, including our over-burdened hospitals, and improving the health and wellbeing of people in communities everywhere.
‘We look forward to working constructively with the Government, because there is too much at stake to get this wrong.’
At a press conference launching the report, Federal Health and Aged Care Minister Mark Butler said improving access to general practice and primary care, particularly outside usual business hours, is a ‘key message’ that emerged from the Taskforce.
He also referenced the need to provide support for longer general practice consultations and establish ‘sustainable models of care’ in rural and remote areas.
‘This report and the recommendations contained in it will guide the deliberations of Government between now and [the] Budget to frame particular investments needed to deliver our commitment to rebuild general practice and, more broadly, strengthen Medicare,’ Minister Butler said.
‘The report recommends supporting this with new blended funding models, integrated with the existing fee-for-service model, allowing teams of GPs, nurses, midwives, and allied health professionals to work together to deliver the care people need.
‘The Taskforce found that strengthening primary care with a greater range of health professionals working to their full scope of practice will optimise use of the health workforce across a stretched primary care sector.’
In response, the RACGP President reaffirmed the college’s position that any reforms need to reinforce the role of GPs as the custodians of patient care.
‘The report states that responsibility for providing care should be shared across primary care teams and that high-quality primary care depends on harnessing the skills of a diverse health workforce including nurses, nurse practitioners and pharmacists,’ she said.
 RACGP President Dr Nicole Higgins says the report contains many promising elements, but that more action is needed.
RACGP President Dr Nicole Higgins says the report contains many promising elements, but that more action is needed.
‘The devil is in the detail here. If the current model is broken and GPs – the specialists in coordinating complex care, with well over 10 years of training in diagnostics, treatment, and quality care – are no longer at the centre of care management, patient care will be compromised.
‘We need GPs working hand in glove with allied health professionals, pharmacists, and practice nurses, and they should be supported within general practice, with GPs as the stewards of patient care.’
Dr Higgins also raised concerns about the report identifying a ‘strengthened role’ for Primary Health Networks (PHNs) to drive organisational and cultural change.
‘Again, general practice needs to be at the centre of any changes and if you ask many GPs, they will tell you that adding another layer of bureaucracy by further empowering and funding PHNs is not the best solution,’ she said.
Nonetheless, Dr Higgins said the fact that many of the college’s recommendations to the Government featured in the report is something that bodes well for the future of general practice care.
‘Voluntary patient enrolment could well be beneficial for many patients and the college awaits further detail on the proposed model,’ she said.
‘In the United Kingdom, the capitation approach has seen many GPs doing a lot more for less, at the expense of patient care, and that must be avoided at all costs.
‘
We have previously warned in our submission to the Primary Healthcare 10-Year Plan that any voluntary patient enrolment model must be fit-for-purpose for the Australian health system and align with the flexibility required in general practice care.
‘Digital modernisation also holds great promise, and we are keen to work with Government to make sure we get this right, including privacy and security concerns.
‘As the report makes clear, it’s no use having vital patient health information locked away in different information systems and not shared easily – no one wins in that scenario.’
Progress on payroll tax
Aside from reviewing the Strengthening Medicare Taskforce report, National Cabinet also heard from Queensland Premier Annastacia Palaszczuk in regard to her state’s plan to
institute a two-year moratorium on
the collection of payroll tax from tenant doctors.
‘I said that we are planning, and that Queensland’s committed to, doing that amnesty until the middle of 2025,’ she told reporters following the meeting.
RACGP Vice President and Queensland Chair Dr Bruce Willett told
newsGP the move represents ‘a huge win’, but that the college will still push for nationwide exemptions for tenant doctors.
‘This comes as a great relief for GPs. It gives them time to adjust to this changed interpretation of the laws and it’s come at after months of intensive negotiations with the QRO [Queensland Revenue Office], and the Treasurer [Cameron Dick],’ he said.
‘We’re grateful to the Queensland Treasurer for recognising the problem that this is causing for general practices. We now need to
call on the other states and territories to quickly follow suit to provide certainty.
‘The word of caution is that this is just kicking the can down the road – we need a more long-term resolution in the form of an exemption for the tenant doctor arrangements.’
National Cabinet is next due to meet in late April.
Log in below to join the conversation.
National Cabinet reform Strengthening Medicare Taskforce
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?