News
GPs receive millions to further general practice
Professor Jon Emery and Associate Professor Jason Ong speak to newsGP about their respective research.
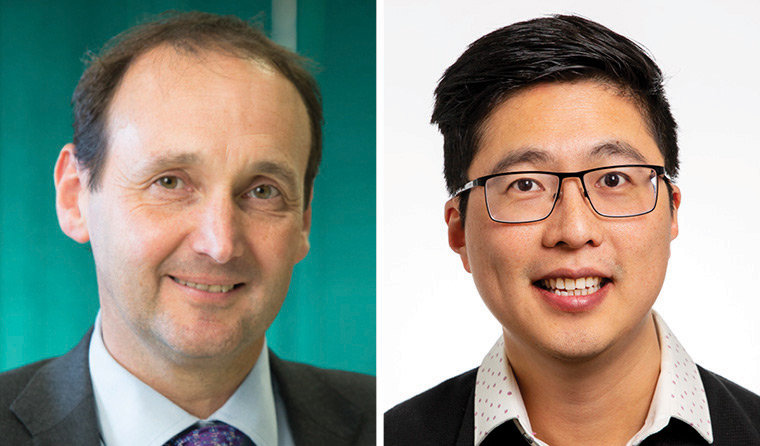 Professor Jon Emery and Associate Professor Jason Ong were both awarded Investigator Grants by the NHMRC.
Professor Jon Emery and Associate Professor Jason Ong were both awarded Investigator Grants by the NHMRC.
Early cancer detection, pharmacogenomic testing for more effective antidepressant prescribing, HIV prevention.
Two GPs have received sought-after grants to conduct research that has the potential to dramatically alter the way healthcare is provided, showing the scope of general practice.
Among the recipients is Professor Jon Emery, GP and Herman Professor of Primary Care Cancer Research at the University of Melbourne and Western Health. He has been awarded a National Health and Medical Research Council (NHMRC) Investigator Grant of $2,360,520 for his project ‘Transforming early detection of cancer in primary care’.
Over five years, the project will seek to transform approaches for the early detection of cancers in primary care through advances in computer-aided diagnosis and use of new genetic tests to identify patients at increased risk of cancer.
‘We know that there are quite a few patients whose cancer diagnosis is delayed, and for a variety of reasons,’ Professor Emery told newsGP.
‘Sometimes it’s by virtue of the nature of the complexity and vagueness of symptoms.’
Professor Emery’s team will draw on data from existing electronic medical records to look at patterns of visits, test results and prescribing in order to develop sophisticated diagnostic algorithms for support tool Future Health Today, which identifies patients that GPs should consider for further investigation.
‘The decision support tool is partly to flag patients who are returning with repeated, but subtle symptoms,’ Professor Emery said.
‘But also, often abnormal test results are not always followed up and some are abnormal results that have only recently been identified as being associated with an increased risk of a cancer diagnosis.
‘Probably the most interesting one is raised platelet count that we know is a marker of a number of cancers.’
The secondary aspect of the project will focus on using genomic testing to assess a patient’s risk of developing bowel cancer over 10 years to then tailor screening tests and prevention.
‘That might prompt GPs to commence screening earlier, for example in their 40s, or potentially to delay screening because they’re actually at lower risk,’ Professor Emery explains.
‘There are a number of polygenic risk scores for a number of other cancers, and we’ll be gradually looking at how you might then start to implement a single test that would actually determine your risk.’
Professor Emery has also been named a recipient of one of 30 Medical Research Future Fund (MRFF) grants, for the sum of $1.39 million, to explore another aspect of genomics.
His team will run a controlled clinical trial, investigating the effects of pharmacogenomics to prescribe antidepressants in primary care for patients with major depressive disorder.
‘It’s been known for some time that there are common genetic variants that determine the way we metabolise a number of different commonly prescribed drugs,’ Professor Emery said.
‘Therefore that affects your responses either in terms of your risk of developing side effects or whether you actually require a larger dose to actually achieve the therapeutic response. Antidepressants are a good example of this.
‘So [it’s] really looking at the impact of using pharmacogenomic tests to tailor both dosage and selection of antidepressant, and the impact that has on resolution of depressive symptoms.’
Associate Professor Jason Ong, a sexual health physician and post-doctoral research fellow at Monash University, was the other GP recipient of an NHMRC grant, receiving more than $1.5 million for his research project ‘Leaving no one behind: community-driven approaches to eliminate HIV in Australia’.
While new HIV infections are declining in Australian-born men, he noted inequities within the statistics that showed numbers on the rise among overseas-born Australian men.
‘A lot of times these people are still “closeted”, so they haven’t come out to their communities and even to GPs they may not identify themselves as gay or at risk for HIV,’ Associate Professor Ong told newsGP.
‘So over the next five years, the project is looking at how we can better serve this group. How do we as the primary care workforce reach these people?’
He believes the missing link in HIV policy is direct community input, which he will seek to obtain through his project using the methodology of crowdsourcing.
‘It’s basically the idea of getting wisdom from the crowds. We get ideas from the affected community and then we develop those ideas rather than imposing certain policies,’ Associate Professor Ong explains.
Through the project, he will also seek greater community involvement when it comes to testing for sexually transmitted diseases (STDs) through the application of a ‘Pay It Forward’ system, which Associated Professor Ong successfully trialled in China.
‘It usually costs about US$22 to do a test, which is very expensive for the Chinese. So we ran a trial where told patients “You can actually test for STDs for free. Because someone cares for you, they paid for you”. Then after they’ve done the test, we give them the option “Do you also want to pay it forward?”,’ he said.
‘The theory is that if it does work, it kind of goes viral and people just pay for each other.
‘I’ll be using activities like this, trying to get the community to also participate, rather than doctors just saying that you should do an HIV test.’
It was while working as a general practice registrar at a clinic focusing on sexual minorities that Associate Professor Ong’s interest in sexual health developed.
‘I never really thought about that as GP, but it certainly sparked some interest in how there are quite specific needs in that population, but also there are ways that GPs can provide that holistic care,’ he said.
‘That’s the strength of a GP – it’s not just talking about sexual health, it’s the holistic person, dealing with their mental health, substance use, and all sorts of things.
‘In fact, HIV is not diagnosed by the specialists, it’s actually the GPs that diagnose most of the HIV cases in Australia. So there’s a need to harness this workforce and also get them to think outside the box.’
While the majority of healthcare is delivered through general practice, with 84% of the population seeing a GP at least once each year, a much smaller proportion of NHMRC funding is allocated to GPs.
As such, Professor Emery says GPs are well placed to provide even greater insights.
‘We also need to be supporting other types of research. Maybe that’s using existing data from general practice so that we really understand what contributes to high quality care where there are potential evidence gaps in the way that care is being provided,’ he said.
‘That requires us to be supporting this concept of practice-based research networks.’
Log in below to join the conversation.
cancer general practice research HIV mental health NHMRC Investigator Grants sexual health
newsGP weekly poll
Which of the following areas are you more likely to discuss during a routine consultation?