News
‘We are heading for a crisis’: Can GP home visits be revived?
They used to be a staple of general practice, but home visits have more than halved in recent years. GPs give their take on the situation.
 Home visits used to be part of the weekly routine for many GPs, but that has changed in recent years.
Home visits used to be part of the weekly routine for many GPs, but that has changed in recent years.
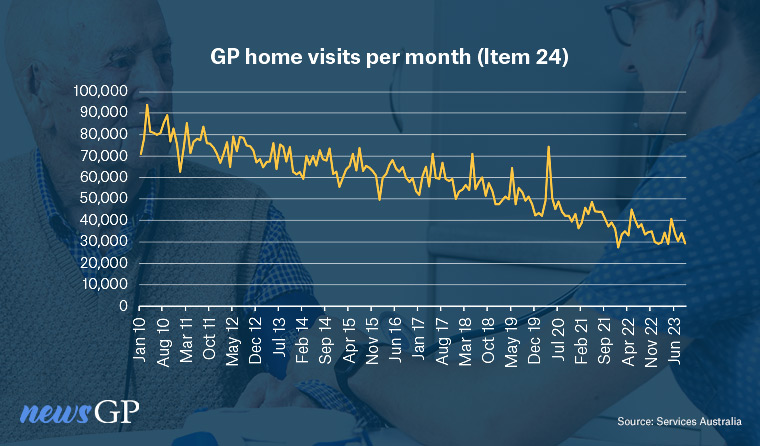
The graph only tells part of the story – but even in raw statistical terms, the change is dramatic.
A decade ago, more than 70,000 MBS item 24s – the most common Medicare rebate reimbursing the extra costs of a home visit – were used every month. Now that number stands at just above 30,000.
As for the human impact behind those statistics, Adelaide-based GP Dr Daniel Byrne understands that well.
The former Chair of RACGP SA&NT, he once regularly went on home visits but that has changed in recent years.
‘Even 30 years ago, it was a service that you did for your practice patients,’ he told newsGP.
‘You didn’t make money out of it.
‘I used to take a lot of palliative care patients on referral from the public system, when they didn’t have a usual GP that would do home visits.
‘I used to enjoy that work but it just became nonsensical. I can’t do a home visit cost effectively.’
Now Dr Byrne only visits long-established patients for palliative care treatment, and notes that for many younger GPs, home visits are simply not part of the work routine.
‘There’s one doctor who does a few like me, but she’s retiring,’ he said.
‘It’s all of us who are older – we were trained, we grew up with a home visit round.’
Associate Professor Joel Rhee, Chair of RACGP Specific Interests Cancer and Palliative Care, shares Dr Byrne’s concerns about the decline, describing it as ‘a huge problem’.
While he believes there are several factors behind it, Associate Professor Rhee pinpoints rebate stagnation as the most significant and notes the impact on two groups in particular: older patients who find travel difficult, and those who need palliative care.
‘Of course, patients can be privately billed, but many patients are not able to afford this,’ he told newsGP.
‘The most vulnerable members of our community including those with palliative care needs may miss out on care, suffer from unmet care needs, and could end up having to call an ambulance and requiring hospital admission.’
He acknowledges telehealth offers more options for home-bound patients, but Associate Professor Rhee says many of those unable to attend practices are likely to have complex conditions, increasing the challenges of providing treatment without face-to-face contact.
‘The GP cannot even bill a telehealth/telephone item number for a patient that they, or another doctor at the practice, have not seen in person in the previous 12 months,’ he said.
‘There is an urgent need for the Government to invest in home visits.’
Increasing need
One GP with a deep understanding of both the challenges and rewards of home visits is Professor Geoff Mitchell, who won a lifetime achievement award at this year’s National Palliative Care Awards.
A long-term GP, and Emeritus Professor of the University of Queensland Medical School, Professor Mitchell sees the decline as a pressing issue that needs to be addressed.
‘The reduction in house calls is quite dramatic and a real problem given that the need for them is increasing,’ he told newsGP.
The trebling of the bulk billing incentive, which came into force this month, will help according to Professor Mitchell. Item 24 is covered under the new set-up, but he believes it will need to be adjusted for inflation in the future to keep making a difference.
He also makes a distinction between rare home visits for people nearing the end of their lives, and regular home visits for other patients.
‘For people who can’t get out of their homes but are not palliative, you might be signing up for a commitment for years,’ he said.
‘Again, the only economic way of managing this is in your own time.
‘You might do that for a handful of people, but for a substantial number, the economics do defeat you.’
He notes the more challenging travel logistics in remote areas, and other factors that influence how frequently visits can take place, including the changing nature of general practice business.
‘Corporate practices by and large look very closely at maximising profits for the owners, and house calls can be actively discouraged,’ he said.
Changing demographics, with younger GPs often combining work with care responsibilities, also play a part in squeezing the capacity for home visits, Professor Mitchell says.
Other doctors fear of being out of their depth, particularly for palliative care, or overseeing the use of opioids, he believes.
Echoing concerns raised by Dr Byrne, Professor Mitchell believes house calls are becoming something of ‘a foreign concept’ for many of those coming through the general practice ranks.
That is not the case for everyone, however.
Dr Natasha Nogueira works for Banksia Medical Centre – recently named the General Practice of the Year in the RACGP awards – out of their Torquay clinic, and regularly carries out home visits.
Having trained in Brazil, Dr Nogueira is now an RACGP Fellow and embraces the variety of the job.
She has observed that for some GPs going outside of the consulting room is not their ‘cup of tea’, and that safety can be a concern for some, depending on the individual doctor and the areas where they work.
However, for Dr Nogueira the experience has been positive, and as Dr Byrne suggested, it is partly down to a question of habit.
‘For me, it has always worked really well,’ she told newsGP.
‘I come from a background that I am used to doing home care in Brazil, like hospital in the home for complex patients, so I’ve always been more mobile than other doctors, that has always been my nature.
‘I absolutely love it. If I could choose I would do it for four days a week, five days a week.’
However, she describes bulk billing as ‘pretty much impossible’ to do, saying there is a lone bulk billed patient on her rounds.
Looking ahead
To boost home visits, the GPs interviewed agreed that an increased rebate to match the call-out fee for aged care home residents would make a difference.

Dr Daniel Byrne is concerned about the decline in home visits carried out by GPs.
For Professor Mitchell, the most important change would be to instil a culture of home visits in GPs during training.
Dr Byrne says he remains hopeful the home visit culture he once knew can be revived, but he also sounds a warning.
‘It will require a major paradigm shift from the Federal Government,’ he said.
In response to a newsGP inquiry about home visits and any initiatives to address the decline, the Department of Health and Aged Care noted that additional MBS item numbers for Level E consultations lasting more than an hour started on 1 November. These cover care outside of consulting rooms, including home visits.
The spokesperson acknowledged the decline of item 24 but said telehealth may be an appropriate substitute in some circumstances.
‘It is a matter for the patient and medical practitioner to determine the appropriate mode of consultation,’ they stated.
‘As part of the ongoing continuous review of the MBS, the department will continue to look at options which support the availability and appropriate use of home visits.’
Professor Mitchell would like to see those choices expanded and nuanced.
‘Home visits for palliative care could attract an incentive or a new set of items could be generated that recognise the inherent complexity of these visits,’ he said.
‘Palliative care, and aged care, gets easier the more you do. If a GP avoids it when they are young, they won’t do it as their patients grow older.
‘We have a rapidly growing older population who will have chronic disease and who will die.
‘As a result, we are heading for a crisis. The solutions for this need to be enacted now.’
Log in below to join the conversation.
home visits item 24 palliative care
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?