News
General practice summit: ‘We have a crisis on our hands that is incontrovertible’
RACGP leadership and healthcare stakeholders gathered at Old Parliament House for a ‘unique opportunity’ to establish solutions to ensure general practice sustainability.
 RACGP President Adjunct Professor Karen Price addresses the media.
RACGP President Adjunct Professor Karen Price addresses the media.
‘This is a crisis, and something I’ve never seen before in my time of 30 years in general practice, of GPs everywhere feeling that their work is unsustainable.’
That is RACGP President Adjunct Professor Karen Price, addressing media at the college’s General Practice Crisis Summit at Old Parliament House in Canberra on 5 October.
The event was called to gather general practice leaders and healthcare stakeholders to discuss the future of general practice and establish solutions for reform.
‘We’ve got doctors who are looking for other employment or to wind down hours, and we’ve got doctors at the end of their careers looking to bring forward their retirement,’ Professor Price said.
‘This is a crisis and we know that Australia is in danger of running out of GPs.’
The RACGP is calling for Federal Government action on three key policy areas, which are the focus of the summit’s working group discussions:
- Funding models
- Strengthening the workforce
- Data governance
‘These issues have caused a lot of discussion among the general practice community and I have been asked non-stop to please deliver this [summit and outcomes via the White Paper], as GPs are desperate,’ Professor Price said.
‘General practice is the best medical specialty because you get to have a longitudinal relationship with your patients, and that came out clearly in the
2022 Health of the Nation report – that despite this crisis, there is a paradox that 70% of GPs are very satisfied with their job.
‘But we have [only] 7.4% of the health budget that goes to general practice – and that must change. We need to have a coordinated health system.’
Professor Price is calling for one health system, where states and territories contribute to primary care to aid coordination across jurisdictions and prevent healthcare from being used as a ‘political football’ between federal and state jurisdictions.
‘We also need to reduce the amount of red tape, because this is really strangling general practice. It’s causing people to under-charge and to do the work but not be paid for it,’ she said.
‘That’s causing a great feeling of disrespect among GPs … and angst in the community.’
Dr Sarah Chalmers, President of the Australian College of Rural and Remote Medicine, and Professional Services Review Acting Director and AMA representative, Dr Antonio Di Dio, echoed Professor Price’s calls for urgent reform to current funding models.
Dr Chalmers highlighted the workforce shortages in rural and remote communities.
‘This has been our significant issue for quite some time, and putting that simply, we do not have enough doctors working in rural and remote Australia … GPs need to have an extended scope of practice,’ she said.
‘The narrative has been degraded to this point in time, when medical students don’t see general practice as an attractive career. Once we get them, there are some great training pathways to encourage doctors to stay in rural and remote areas.’
GP Dr Mukesh Haikerwal, Master of Ceremonies for the event, told reporters the summit will allow key leadership to explore answers for the issues facing general practice.
‘We need to have the right solutions, the right ideas and make sure that we have a common voice within this meeting,’ he said.
‘Addressing general practice needs to be of great magnitude to determine the future of Australia’s healthcare.
‘How [can] we reorganise the divisions of health for a better country?’
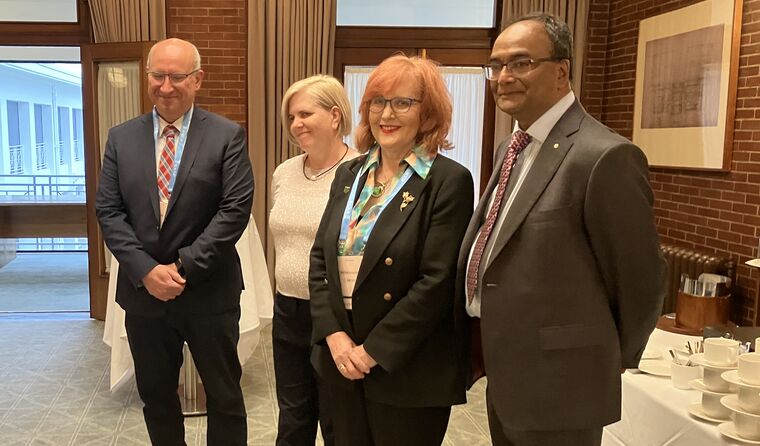 (From L–R) AMA representative and Professional Services Review Acting Director Dr Antonio Di Dio, ACRRM President Dr Sarah Chalmers, RACGP President Adjunct Professor Karen Price and summit MC Dr Mukesh Haikerwal.
(From L–R) AMA representative and Professional Services Review Acting Director Dr Antonio Di Dio, ACRRM President Dr Sarah Chalmers, RACGP President Adjunct Professor Karen Price and summit MC Dr Mukesh Haikerwal.
Following the pre-event press conference, Dr Haikerwal officially opened the General Practice Crisis Summit after an Acknowledgement of Country from
Associate Professor Brad Murphy.
‘General practice is in crisis – we can’t turn a blind eye, it is the cornerstone of the health system, linking all care,’ Dr Haikerwal said.
‘We know the system must be transformed. General practice is ideally placed to understand what the current healthcare system is, where it’s failing and to help meet the needs of Australians.
‘Today is a unique opportunity to come together with proposed innovative solutions for ensuring general practice sustainability and providing the best patient outcomes, starting with access and affordability.’
Dr Haikerwal said while a long-term plan is required, ‘immediate action’ is also needed to ease the pressure on an already crumbling system.
Professor Price followed with a keynote presentation outlining why general practice in Australia is at ‘breaking point’, pointing to the current key issues of insufficient Medicare rebates and the closure of many general practices, particularly in rural and remote areas.
‘Rural general practice is the canary in the coalmine,’ she said.
‘General practices are being forced to close, [for example] we’ve had the
TriStar collapse and more
Queensland practices closing. This is a manufactured tragedy that didn’t have to happen.
‘We are fighting for patients … and the newly released Health of the Nation report has made it very clear that we have a crisis on our hands that is incontrovertible. The pipeline is leaking from the beginning, the middle and the end.’
With access to general practice undervalued, Professor Price believes the profession has been disrespected and ‘grossly underfunded for decades’, while GPs’ workload has increased.
‘The good GP is invisible,’ she said.
Federal Health and Aged Care Minister Mark Butler also provided a pre-recorded video. He said the Government looks forward to working closely with the college to strengthen Medicare and Australia’s primary care system.
‘Every day, everywhere I go, people talk to me about how it’s getting more and more difficult to see a doctor,’ Minister Butler said.
‘And this is why as a government, we’re committed to working with the primary care sector to strengthen Medicare, and to make it easier for Australians to access their local GP and other healthcare professionals.
‘Without this, it’s going to get even harder to see a GP and the out-of-pocket expenses will only increase. Importantly, it’s only through fixing primary care that we will take the pressure off our overburdened hospitals.
‘Australians trust their GPs. You’re the backbone of our primary care system. It’s through the vital relationships that you have with your patients that ensures all Australians can get the quality health care they deserve.’
Professor Price concluded the presentation by thanking attendees, highlighting that without general practice, the entire health system will fail.
‘General practice provides 177 million services a year to approximately 24 million people in Australia,’ she said.
‘And that’s why we called the crisis summit today, to talk about solutions and to deliver a White Paper.
‘We have, thankfully, patient representatives here today, we have leaders from general practice, GPs from the frontlines, international medical graduates, academia, and many of our local allies and non-GP allies here to develop solutions.
‘I really do truly want to thank you very much for uniting behind this really important cause. We need solutions to rethink the way things are being done.
‘We want to work together to ensure the absolute best possible outcome for all our communities across the country.’
The outcomes from the three key working group discussions will be published on newsGP on 6 October. The proposed solutions from the summit will be released to Government in a White Paper in the coming weeks.
Log in below to join the conversation.
Canberra General Practice Crisis Summit general practice funding government investment
newsGP weekly poll
How often do patients ask you about weight-loss medications such as semaglutide or tirzepatide?