News
COVID-19 vaccination gap ‘a national shame’
The RACGP has raised concerns over the gap in vaccine coverage between Aboriginal and Torres Strait Islander people and non-Indigenous Australians.
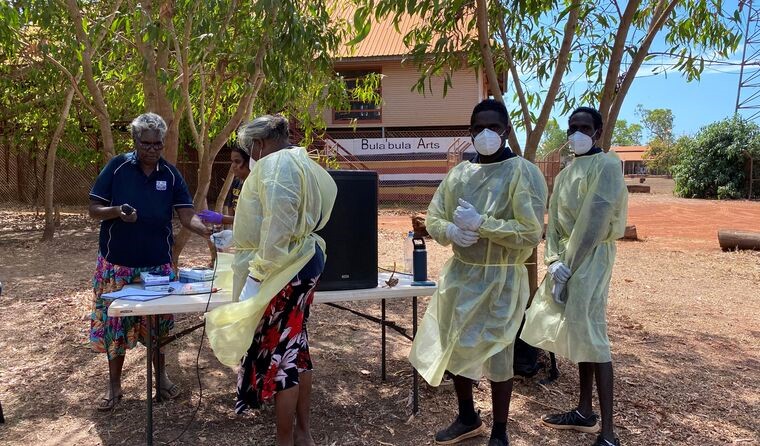 Nationally, the gap between double dose vaccination rates in the general population and Aboriginal and Torres Strait Islander people is just over 26%. (Image: NAACHO)
Nationally, the gap between double dose vaccination rates in the general population and Aboriginal and Torres Strait Islander people is just over 26%. (Image: NAACHO)
When Australia’s vaccine rollout commenced in February, Aboriginal and Torres Strait Islander people were among the first to be eligible.
The decision was strategic. Given the health inequities and higher rates of chronic disease, all insight about COVID-19 indicated that Aboriginal and Torres Strait Islander communities would be at higher risk of severe disease and death should the virus spread.
But nine months on, and with the focus now firmly set on easing public health measures as the country eclipses its vaccine targets, the gap in vaccine coverage between Aboriginal and Torres Strait Islander people and non-Indigenous Australians is stark.
As of Tuesday 9 November, 81.1% of Australians aged 16 and over are fully vaccinated, with 89.5% having received at least one dose, but just 54.5% of Aboriginal and Torres Strait Islander people aged 16 and over are fully vaccinated, with 66.2% having had one dose.
In certain jurisdictions, the disparity is even more striking.
In New South Wales, Victoria and the Australian Capital Territory, where outbreaks and prolonged lockdowns have taken a toll, just over 70% of Aboriginal and Torres Strait Islander people are fully vaccinated and 80% have had a first dose, while the first dose rate sits below 55% in the largely COVID-free states of Queensland, South Australia and Western Australia.
That is despite a vaccination surge plan, announced in September, to increase coverage across 30 Aboriginal communities throughout the country.
Professor Peter O’Mara, a Wiradjuri man and Chair of RACGP Aboriginal and Torres Strait Islander Health, has grave concerns as Australia moves to living with COVID-19.
‘We are going to see many more positive cases,’ he said.
‘The fact that there remains a serious gap in vaccine coverage between Aboriginal and Torres Strait Islander people and non-Indigenous people in this country is a national shame.’
Cherbourg, a town located just over three hours’ drive from Brisbane where more than 98% of the population identifies as Aboriginal, is the local government area with the lowest vaccination rates in the country with just 27.2% of those aged 15 and over fully vaccinated, and 39.5% having had at least one dose, as of 8 November.
A similar trend is seen in Yarrabah in Far North Queensland. More than 97% of the population identifies as Aboriginal and/or Torres Strait Islander, and just 29.8% have received two doses and 50.7% have received one.
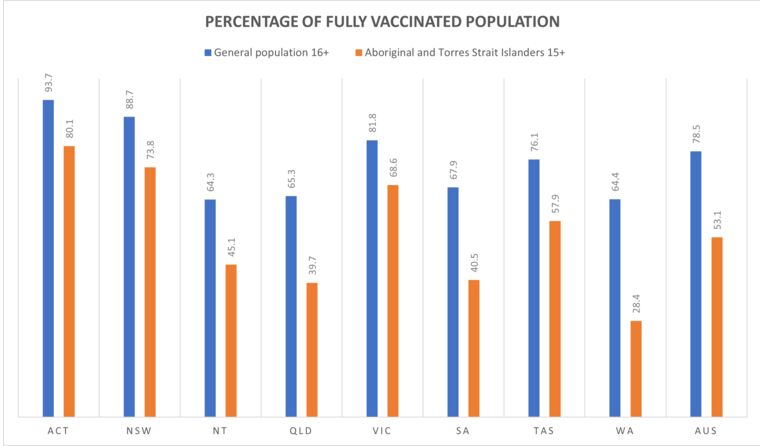 The percentage of non-Indigenous Australians aged 16 and over, and Aboriginal and Torres Strait Islander people aged 15 and over, who are fully vaccinated as of 3 November.
The percentage of non-Indigenous Australians aged 16 and over, and Aboriginal and Torres Strait Islander people aged 15 and over, who are fully vaccinated as of 3 November.
Despite the relatively successful efforts made at the start of the pandemic to keep the virus out of vulnerable communities, Aboriginal and Torres Strait Islander people have been disproportionately affected since Delta became the dominant strain.
Aboriginal and Torres Strait Islander people in NSW and the ACT have been affected at twice the rate of non-Indigenous Australians, accounting for 10% of all COVID-19 cases.
‘In only the past three months there have been more than 7000 cases among Aboriginal and Torres Strait Islander peoples, with over 700 people hospitalised including 80 ICU admissions and 16 deaths in New South Wales, Victoria and the ACT,’ Professor O’Mara said.
However, it was just last month that COVID-19 Taskforce Coordinator Lieutenant General John Frewen said that the Federal Government had ‘no specific timeline’ to close the gap in vaccination coverage, citing key challenges ranging from hesitancy to misinformation and complacency.
But with Christmas little more than a month away and travel to rural parts of the country expected to ramp up, Professor O’Mara believes there is urgent need to focus on increasing vaccine access and education.
‘While the tourism is needed, it brings enormous risk to communities not protected by vaccination,’ Professor O’Mara said.
‘So as we move to enjoying more freedoms, it’s critical that we do more to achieve high rates of vaccination among Aboriginal and Torres Strait Islander people across the country – we cannot leave anyone behind.
‘This requires working together with communities and leaders to tackle the scourge of health misinformation and ensure messages about the importance of vaccination and COVID-safe practices reach everyone.’
Professor O’Mara praised the early community-led action taken to limit the impact of the pandemic on Aboriginal and Torres Strait Islander communities, saying that Australians ‘should be proud’, but warned that ‘we are far from out of the woods’.
‘We need to knuckle down and work together to improve access to care for appointments missed, and boost vaccination rates and measures to ensure the protection and health of our communities,’ he said.
Log in below to join the conversation.
Aboriginal and Torres Strait Islander health COVID-19 telehealth vaccines
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?