News
Antibiotic prescribing down but ‘superbug’ threat remains
Antimicrobial resistance remains an ongoing risk to patient safety despite GPs leading the charge against antibiotic overuse, a new report has found.
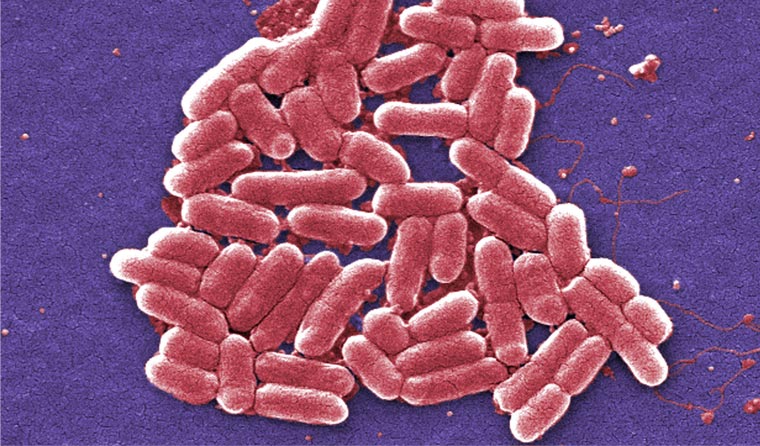 The continued inappropriate levels of antibiotic prescribing risks are creating ‘superbugs’. (Image: Centers for Disease Control)
The continued inappropriate levels of antibiotic prescribing risks are creating ‘superbugs’. (Image: Centers for Disease Control)
The Antimicrobial use and resistance in Australia 2019 (AURA 2019) report states that overall antibiotic use in the community has dropped for the first time in 20 years, a reduction partly attributed to coordinated campaigns targeting GPs and consumers on the risks of using antibiotics inappropriately.
RACGP President Dr Harry Nespolon described the results as ‘a good start’ and told newsGP that he is encouraged by the downward trend.
‘General practice is again leading the way, but we need to remain conscious of this issue all the time and keep improving the way we prescribe antibiotics,’ he said.
‘It’s good to see that there’s been expanded surveillance … [and] it’s important that in the areas where we are using broad spectrum antibiotics that continued surveillance occurs.’
Dr Nespolon added that the report’s findings also support RACGP efforts to limit the number of professionals able to prescribe antibiotics to the general community.
‘It just underlines our campaign to not have other prescribers, including pharmacists, prescribing antibiotics,’ he said.
‘It shows that the decision by the NSW Health Minister is a correct one and the evidence shows that this approach is much better than the Queensland approach.’

RACGP President Dr Harry Nespolon said he is encouraged by the downward trend in antibiotic prescribing, but doctors need to ‘remain conscious of this issue all the time and keep improving the way we prescribe antibiotics’.
But despite the downward trend, antibiotics continue to be overprescribed compared with guideline recommendations. The report warns that antimicrobial resistance shows little sign of abating and poses an ongoing risk to patient safety.
Professor Danielle Mazza, co-author of the RACGP’s Response to antimicrobial resistance in primary care, told newsGP that increased focus on general practice in the area of antimicrobial stewardship would represent a positive step towards combatting the problem.
‘It’s comforting that there is starting to be a decline, but clearly lots more work needs to be done and the issues raised in the RACGP position statement remain very relevant,’ she said.
‘We need a framework to support general practice antimicrobial stewardship that looks at the wide range of issues impacting on antibiotic prescribing in general practice; from governance and regulation, to involvement of pharmacists, to regular audit and feedback, provision of resources and better training for GPs.
‘We also need improvements to medical software to be able to link prescribing to the reason why you’re doing it so better audits can be done.
‘It’s about being able to look at the reason for prescription and ensure that there is better guideline concordance. That’s the big gap in general practice.’
According to Professor Mazza, most of the emphasis to date has been on hospital prescribing, and data sources for antimicrobial stewardship in primary care remain limited, which is insufficient to provide a deep insight into antibiotic prescribing, particularly at a regional level.
‘The majority of antibiotic prescriptions occur in the community,’ she said.
‘Government really has to, in conjunction and consultation with the RACGP and other relevant organisations, address the complexity of issues affecting antimicrobial stewardship in general practice and provide funding and initiatives related to all of those areas.
‘There is wide recognition of the problem, I just don’t think there has been adequate focus on it.’

Professor Danielle Mazza believes an increased focus on general practice in the area of antimicrobial stewardship would represent a positive step towards combatting the problem of resistance.
The report found that in 2017 more than 10 million Australians had at least one antibiotic dispensed in the community and more than 26.5 million prescriptions for antimicrobials were dispensed overall. However, AURA Clinical Director Dr Kathryn Daveson said more work needs to be done.
‘While the downward shift in prescribing will help to slow the spread of resistance, these latest AURA findings indicate that the levels of inappropriate prescribing of antibiotics in hospitals and the community are still too high,’ she said.
‘AURA 2019 also identifies focus areas that need increased attention, including reducing inappropriate prescribing of broad spectrum antibiotics, particularly for urinary tract and skin infections; and improving the appropriateness of antibiotic prescribing for chronic obstructive pulmonary disease and other respiratory infections.’
Labelled by the Australian Commission on Safety and Quality in Health Care as the ‘most comprehensive’ report ever produced on Australian antimicrobial use and resistance trends, the data also highlights common pathogens such as E. coli, Salmonella, Neisseria gonorrhoeae and Neisseria meningitidis that are reportedly becoming increasingly resistant to major drug classes.
Additionally, some organisms are now resistant to last-resort treatments, and Professor Mazza called on government bodies such as the Medical Research Future Fund and the National Health and Medical Research Council to provide calls for targeted research in general practice to combat the growing problem.
‘It’s a critical issue because of the rising rates of antimicrobial resistance and the threat of a future where we have very limited antibiotics to treat infections,’ she said.
‘Hopefully there are some clever people working in laboratories that will find new approaches but, at the moment, the outlook is pretty gloomy.’
Some key findings on antimicrobial use from AURA 2019:
- In 2017, 41.5% of the Australian population had at least one antimicrobial dispensed.
- The overall rate of inappropriate prescribing of antimicrobials in Australian hospitals that contributed to the National Antimicrobial Prescribing Survey (NAPS) has been static since 2013. In 2017, 23.5% of antimicrobial prescriptions assessed were found to be inappropriate.
- Antibiotics used in surgery (surgical prophylaxis) are often not required and are given for too long. The proportion of prescriptions for surgical prophylaxis that extended beyond the recommended 24 hours dropped in NAPS contributor hospitals from 41.1% in 2013 to 30.5% in 2017.
- Cefalexin and amoxicillin–clavulanic acid had the highest rates of inappropriate prescribing in NAPS contributor hospitals.
- After a steady increase in the rate of antibiotic dispensing under the Pharmaceutical Benefits Scheme (PBS)/Repatriation Pharmaceutical Benefits Scheme (RPBS) between 2013 and 2015, there was a decline in 2016, and a further decline in 2017.
- This decline was also seen in participating MedicineInsight practices since 2010. In 2017, 26% of patients from participating MedicineInsight practices were prescribed systemic antibiotics; however, antibiotics continue to be overprescribed compared with guideline recommendations.
- A large percentage of patients from participating MedicineInsight practices were prescribed antibiotics for conditions for which there is no evidence of benefit, including influenza (52.2% of patients with this condition recorded) and acute bronchitis (92.4% of patients with this condition recorded).
- The mostly commonly supplied antibiotics under the PBS/RPBS continue to be cefalexin, amoxicillin and amoxicillin–clavulanic acid.
- Approximately 50% of all antibiotic prescriptions in the community were ordered with repeats; of those repeats, approximately half were filled within 10 days of the original prescription.
- There is a high rate of use of antimicrobials for unconfirmed infections in aged care homes that participated in the Aged Care National Antimicrobial Prescribing Survey (AC NAPS). More than half of antimicrobial prescriptions were for residents who had no signs or symptoms of infection.
- Approximately one-quarter of prescriptions in 2016 and 2017 in aged care homes that participated in the AC NAPS did not include the reason for prescribing antimicrobials.
- Approximately one-third of antimicrobial prescriptions in 2016 and 2017 in aged care homes that participated in the AC NAPS were for topical use.
antibiotics antimicrobial resistance bacteria superbugs
newsGP weekly poll
As a GP, would you benefit from further education about identifying and supporting patients impacted by intimate partner violence?