News
Calls to list drug-resistant fungus as a notifiable disease
Candida auris is persistent, deadly, and may be fuelled by climate change.
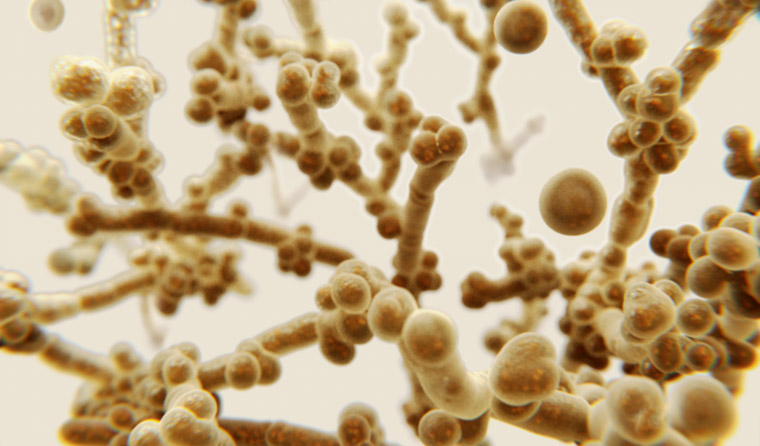 Candida auris developed resistance to many common anti-fungal agents, including fluconazole.
Candida auris developed resistance to many common anti-fungal agents, including fluconazole.
Ten years ago, an unusual fungus was isolated on the ear of a 70-year Japanese woman.
Part of the yeast genus, it was named Candida auris – Latin for ear.
It initially seemed a novelty – a new yeast that lived on the skin. Two years later, however, the first cases of related infection emerged in South Korea.
Doctors soon found that the fungus became very dangerous if it invaded the bloodstream. Patients with weakened immune systems had a 30–60% chance of dying from the infection.
And unlike many other fungal infections, this one could spread from person to person.
Worse still, the fungus had developed resistance to many common anti-fungal agents, including the traditionally dependable fluconazole.
Hospitals where Candida auris has taken root have had to take serious measures to eradicate it. One British ICU had to temporarily close after the fungus swept through. Doctors and nurses asked to work with infected patients reported major concerns for their own safety.
Its persistence and potential lethality has rocketed Candida auris to prominence as a drug-resistant superbug. An added challenge is the fact it is often misidentified as a common yeast infection in pathology labs.
The threat has led a leading superbug expert – who has seen the impact of the fungus firsthand in the US – to call for Australia to urgently list the fungus on the National Notifiable Diseases List (NNDL), as has been done in the States.
Dr Marion Kainer, Tennessee’s former infectious diseases director, said several cases have already been reported in Australia.
‘[A]s it is not a nationally notifiable germ, it may be underappreciated as a threat,’ she said.
Dr Kainer, now the head of infectious diseases at Western Health in Victoria, described the fungus as ‘really unusual.’
‘Candida does not usually cause outbreaks; it does not normally spread person-to-person,’ she said. ‘You want to contain a spark before it becomes a raging bushfire.’
Victoria will be the first Australian state to list the fungus as a notifiable disease early next year.
A Department of Health spokesperson told newsGP no jurisdiction has requested the listing of Candida auris on the NNDL.
‘Whilst individual jurisdictions collect data on Candida auris, it is not currently a nationally notifiable disease,’ the spokesperson said.
As of this year, the fungus is being monitored through the National Alert System for Critical Antimicrobial Resistance, which is part of the Australian Commission on Safety and Quality in Health Care.
The new National Antimicrobial Resistance Strategy, to be launched next year, will also consider Candida auris as part of a broader focus on resistant fungi, the spokesperson said.
Events overseas have heightened concerns regarding the pervasiveness and danger of the fungus.
An older American man was diagnosed with invasive Candida auris in May 2018. He died 90 days later – but the fungus did not, as the New York Times reported.
The fungus was so invasive, ceiling and floor tiles had to be removed from the hospital in which the man was treated, and special cleaning equipment used. The normal disinfectants had no effect.
‘Everything was positive, the walls, the bed, the doors, the curtains, the phones, the sink, the whiteboard, the poles, the pump,’ the hospital’s president told the paper.
‘The mattress, the bed rails, the canister holes, the window shades, the ceiling, everything in the room was positive.’
Connecticut deputy state epidemiologist Dr Lynn Sosa told the New York Times she now saw Candida auris as the top threat among resistant infections.
‘It’s pretty much unbeatable and difficult to identify,’ she said.
After its isolation in 2009, samples of the fungus were found in hospital patients from India, South Africa and Venezuela – representing three separate continents.
Genetic analysis found each clade was distinct. That suggested the fungus had emerged near-simultaneously in multiple locations.
Researchers from Johns Hopkins Bloomberg School of Public Health studied the puzzling fungus and concluded in an mBio paper that climate change might be playing a role in its rapid emergence into more than 30 countries.
They found Candida auris was better adapted to growing at higher temperatures than its close relatives, and posit that as temperatures rise the thermal gradient that has historically given humans significant protection against fungi will reduce.
‘[T]here is concern that higher ambient temperatures will lead to the selection of fungal lineages to become more thermally tolerant, such that they can breach the mammalian thermal restriction zone,’ the paper states.
‘[C]apacity for virulence is a complex property that emerges from many attributes, and it is improbable that it would have occurred concurrently on three continents, unless driven by another factor that selected for it.’
Dr Arturo Casadevall, lead author of the paper and Chair of the Department of Molecular Microbiology and Immunology sees a genuine threat as global temperatures continue to rise.
‘We are very remarkably resistant to fungal diseases. The reason for that is because we have advanced immunity and [a] high temperature,’ he told Infectious Diseases News. ‘The combination of the two gives us phenomenal resistance because most fungi cannot grow in mammalian temperatures.
‘But what would happen if more began to adapt to higher temperatures?
‘That is, to me, the threat.’
Other researchers have suggested anti-fungal use in agriculture may contribute, citing another fungus Aspergillus, which developed resistance to itraconazole – medication very similar to azole pesticides.
Log in below to join the conversation.
antimicrobial resistance candida auris drug resistance fungi
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?