News
AstraZeneca and Pfizer: What are the side effects of Australia’s vaccines?
People under 55, women and those previously infected with COVID-19 are more likely to report side effects after receiving either vaccine, according to new research.
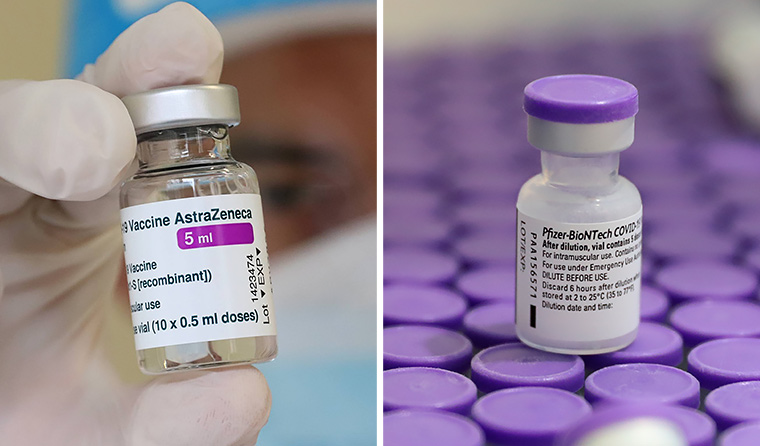 Among recipients of the AstraZeneca and Pfizer vaccines, two in three report local side effects and one in four report systemic effects.
Among recipients of the AstraZeneca and Pfizer vaccines, two in three report local side effects and one in four report systemic effects.
It has been five months since the first vaccine against COVID-19 was administered to a 90-year-old woman in the UK.
Since then, more than one billion doses have been administered worldwide.
Now a new observational study from the UK, published in The Lancet, is giving insight into the typical side effects of the AstraZeneca and Pfizer vaccines, in addition to their effectiveness, in a community setting.
Researchers had 627,383 people self-report their symptoms on the COVID Symptom Study app between 8 December and 10 March after receiving either their first or second dose of the Pfizer vaccine, or their first dose of AstraZeneca.
They found local side effects (pain, swelling, redness, itching, swollen armpit glands) affected two in three people, and were more common in Pfizer recipients. At least one symptom was reported by 71.9% of individuals after the first dose of Pfizer, 68.5% after the second dose, and by 58.7% after the first dose of AstraZeneca.
Systemic side effects (diarrhoea, fatigue, headache, chills, nausea) affected fewer than one in four people, but were more common with AstraZeneca, with at least one symptom reported by 33.7% after the first dose, compared to 13.5% and 22% after the first and second respective dose of Pfizer.
The most frequently reported local side effects were tenderness and pain around the injection site, occurring most often the day after injection. Fatigue and headaches were the most commonly reported systemic side effects, frequently reported within the first 24 hours after vaccination.
The study also tested whether adverse effects varied across individuals’ characteristics, such as age and body mass index (BMI), gender, and health status.
It found side effects are more common among women, people aged 55 years or younger, and after a second dose.
For example, 46.9% (AstraZeneca) and 20.7% (Pfizer) of people aged 55 years or younger reported at least one systemic effect after receiving their first dose, compared with 30.7% (AstraZeneca) and 10.6% (Pfizer) of those older than 55.
However, researchers noted that side effects after both types of vaccine occurred at frequencies ‘lower than reported in phase 3 trials’.
‘For example, in phase 3 clinical trials of the BNT162b2 [Pfizer] vaccine, the most common events after the first dose were injection-site pain (71–83%), fatigue (34–47%), and headache (25–42%). However, in our community analysis, less than 30% of users complained of injection-site pain and less than 25% of fatigue and headache after the first dose,’ the authors wrote.
‘Similarly, rates of side effects following the ChAdOx1 nCoV-19 [AstraZeneca] vaccine were lower than expected. The phase 2–3 trial of the ChAdOx1 nCoV-19 vaccine reported systemic adverse effects in 88% of participants aged 18–55 years who received the first injection, whereas we found a lower rate of 33.7% after the first dose in the overall sample and 46.9% in individuals aged 18–55 years.’
Women (16.2%) were also more likely to report adverse effects than men (9.3%) after the first dose of Pfizer, as was the case after AstraZeneca (39.3% women, 26.2% men).
Side effects were also more common among people who previously had COVID-19, with local effects 1.4 times and systemic effects 1.6 times higher after the first dose of AstraZeneca, and 1.2 and 2.9 times higher after the first dose of Pfizer.
‘It is possible, although it remains to be tested, that this increased reactogenicity relates to increased immunogenicity,’ the authors noted.
‘It has been shown that vaccines have increased immunogenicity in individuals with past infection and these people have higher antibody titres than those without previous infection.’
When it came to BMI and reported comorbidities, the researchers said there were some differences, but that it ‘did not make a significant difference’. However, those with a higher BMI were slightly more likely to report a systemic reaction after receiving the Pfizer vaccine.
Overall, the study found most side effects occur within 24 hours of a person receiving a vaccine and that symptoms typically subside within 48 hours.
Researchers also looked at effectiveness of the vaccines and observed a significant reduction in infection risk starting at 12 days after the first dose, reaching 60% for AstraZeneca and 69% for Pfizer at 21–44 days compared with unvaccinated controls.
‘The reduction of infection was lower in individuals older than 55 years than those aged 55 years or younger, in those with one or more comorbidities than in those without comorbidities, and in individuals with a BMI of 30 kg/m2 or higher than in those with a BMI of less than 30 kg/m2,’ the authors wrote.
While the study included a large sample size, the authors acknowledge a limitation in that the findings rely on self-reports, which can introduce ‘information bias, including misclassification, or effect bias exposure’.
In Australia, where 2,254,074 doses have been administered over the course of 10 weeks, 325,533 recipients have responded to an AusVaxSafety survey. More than half (52.4%) have reported an adverse event, the most common being pain at the injection site, and 1.4% reported visiting a doctor or emergency department as a result.
To help speed up the rollout, the National Cabinet last month brought forward the commencement of phase 2a of the vaccine roadmap. As of Monday, people aged 50–70 are eligible to receive AstraZeneca at state, territory and federal vaccination hubs, and from 17 May in general practices.
Some GPs with an excess supply of vaccines have been permitted to bring that date forward, after contacting their primary health network.
The UK study’s release is timely, offering GPs and patients reassurance that side effects are ‘moderate in frequency, mild in severity and short-lived’.
‘Our data could be used to inform people on the likelihood of side effects on the basis of their age and sex and the type of vaccine being administered,’ the authors concluded.
Log in below to join the conversation.
AstraZeneca effects Pfizer rollout side vaccine
newsGP weekly poll
Within general practice, do you think there are barriers to providing flu vaccinations? If so, what are they?