News
Australia on the verge of eliminating cervical cancer thanks to HPV vaccine and screening programs
Cervical cancer is on track to be eliminated as a public health issue by 2020.
 Associate Professor Julia Brotherton believes Australia’s HPV vaccination programs have been normalised and are like a ‘rite of passage’ for girls and boys.
Associate Professor Julia Brotherton believes Australia’s HPV vaccination programs have been normalised and are like a ‘rite of passage’ for girls and boys.
‘It is pretty incredible to see the powerful impact of vaccination and screening projected this way,’ public health physician Associate Professor Julia Brotherton told newsGP.
A research paper published in The Lancet Public Health this week was designed to assess the timeframe in which Australia is likely to meet the World Health Organization’s 2018 ‘Call to action’ to eliminate cervical cancer as a health risk for women.
‘This study uses a complex and well validated modelling platform to project the future incidence of cervical cancer given current HPV [human papillomavirus] vaccine-uptake rates, the move to the nine valent vaccine this year, and the move from Pap testing to HPV testing for cervical screening in Australia,’ Associate Professor Brotherton, one of the paper’s co-authors, said.
The threshold at which cervical cancer meets the definition for a rare cancer is when it reaches an incidence rate of fewer than six cases per 100,000 women.
According to the new study, Australia is very close to reaching this threshold.
‘We will reach the rare cancer threshold very soon, in 2020, and a plausible elimination threshold [fewer than four cases per 100,000 women] shortly thereafter, in 2028,’ Associate Professor Brotherton explained.
‘In the longer term, we will reach rate of fewer than one case per 100,000 in around 2066 if we maintain full screening in vaccinated women.’
These findings show Australia is on target to deliver a world-first result – the elimination of cervical cancer as a health threat for women within a decade. The paper’s results are also a vindication of Australia’s implementation of the human papillomavirus (HPV) vaccination program, which has previously been a focus of controversy.
‘Because this human papillomavirus only infects humans and the vaccine program prevents the spread of the virus, eventually we’ll get rid of it, like we did with smallpox,’ Professor Ian Frazer, a co-creator of the Gardisil HPV vaccine and co-author of the Lancet paper, told Fairfax.
However, the paper’s authors also acknowledge that inequities of access to the HPV vaccine and cervical screening may still apply to certain populations within Australia, and that vigilance must be maintained to ensure the best possible results across the country.
‘It’s vital we remember these low rates can only be achieved if we continue to vaccinate our children and support all women to participate in screening,’ Associate Professor Brotherton said.
‘We need to bring screening to under-screened groups, which include Aboriginal and Torres Strait Islander women, some CALD [culturally and linguistically diverse] women, and women in other marginalised groups or who have experienced sexual or other trauma.
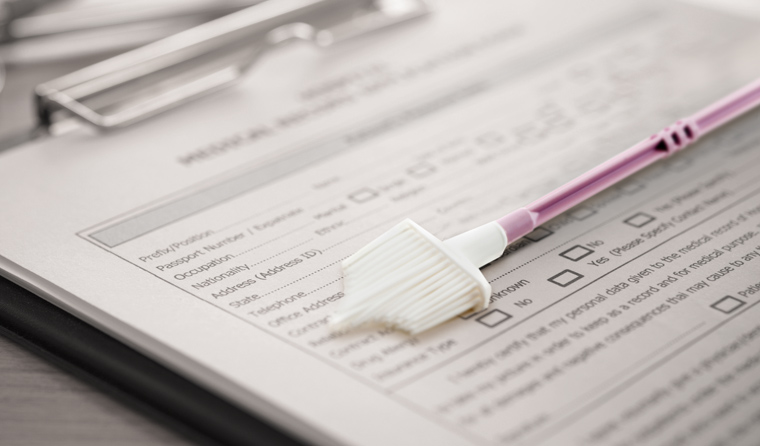
‘Fortunately, cervical screening is now more accessible, acceptable and accurate than ever, with a five-year interval and the option of self-collection for women who refuse a speculum exam and are under or never-screened.’
.jpg.aspx)
Associate Professor Julia Brotherton says the impacts of Australia’s vaccination and screening programs for cervical cancer are ‘pretty incredible’.
Associate Professor Brotherton observes that GPs have played a vital role in reducing cervical cancer by administering and boosting screening and vaccination rates, and outlines three ways in which they contribute to these efforts.
‘Engaging with parents to support HPV vaccination as a normal rite of passage for children when they start high school – every child has the right to the next available cancer protection to optimise their future health,’ she said.
‘Also, speaking with adolescents about whether they did get the HPV vaccine at school. People up to age 19 can receive HPV vaccine under the National Immunisation Program.
‘Finally, supporting the cervical screening program by discussing cervical cancer prevention through screening with their female patients and supporting women’s decision-making around participating in the program.’
The authors of the study also hope its results will encourage other countries to implement and promote their own vaccination and screening programs against cervical cancer, which remains the fourth most frequent cancer among women worldwide, with 90% of deaths occurring in low and middle-income countries.
Associate Professor Brotherton believes Australia’s stunning results offer the rest of the world an inspiring look into a future where cervical cancer need no longer be feared.
‘HPV vaccines are safe, effective and incredibly well-researched, and they now promise to save millions of lives into the future,’ she said.
‘We have the tools to get rates this low and we need to work together to work out how to feasibly deliver them to all.’
cervical cancer cervical cancer screening program HPV vaccine
newsGP weekly poll
As a GP, do you use any resources or visit a healthcare professional to support your own mental health and wellbeing?