News
Calls for GPs to be on high alert for thunderstorm asthma
With asthma-related deaths on the rise, experts have emphasised the need for greater patient education on preventive measures.
 Victoria’s 2016 thunderstorm asthma event saw a 672% increase in respiratory-related presentations at public hospitals.
Victoria’s 2016 thunderstorm asthma event saw a 672% increase in respiratory-related presentations at public hospitals.
When respiratory physician Dr Jonathan Burdon awoke to news of the 2016 thunderstorm asthma event in Victoria – a phenomenon that saw a 672% increase in respiratory-related presentations at public hospitals – he anticipated an influx of phone calls and a queue of patients outside his rooms.
But that influx never came.
‘Over the next three months or so, as patients came through I asked them what they did that night and most of them said they were fine and all of them said, “I did what you told me to do”,’ he told newsGP.
‘And I said, “You mean you take your medication regularly?”. “Yes doctor, and I was a bit wheezy, so I stayed indoors”.’
He says patient education was key.
Australia has some of the highest rates of asthma in the world, with one in 10 people affected.
New data commissioned by the National Asthma Council Australia shows that asthma-related deaths are on the rise, particularly for women and those aged over 75.
There were 421 asthma-related deaths in 2019 – up from 395 in 2018 – consisting of 272 females and 149 males with a rising trend in fatalities for women aged under 54.
‘Women aged under 54 are also usually in the prime of their working life and, when it comes to their health, we know that many women often put the needs of others before themselves,’ Dr Burdon said.
‘This can impact on them making time to visit their healthcare professional, take their medication regularly or make the lifestyle changes necessary to better manage their asthma.’
In addition to having an asthma action plan in place, Dr Burdon says greater emphasis on patient education and preventive measures is also vital to reducing deaths.
‘Where asthma management has gone best is where the patient really understands what the problem is, and why the medicines are being prescribed,’ he said.
‘Make sure that the person with asthma actually understands what asthma is about and that it’s an inflammatory condition, and why in that particular individual their asthma may get worse, and what the common triggers are – for example, pollen, smoke and dust.
‘Then explain what the medicines that are being prescribed actually do, so they get an understanding about why they’re taking their inhalers and what their inhalers contain.’
Dr Burdon says emphasis also needs to be placed on the need to continue to take preventive medicines, even when asthma is under control.
‘We know that a significant portion of people in Australia with asthma prescribed preventive medication don’t take it regularly and they are oversubscribed, if you like, in hospital ICU admissions and in the mortality rate,’ he said.
‘So if you feel okay, it doesn’t mean to say you don’t need to take the medication.’
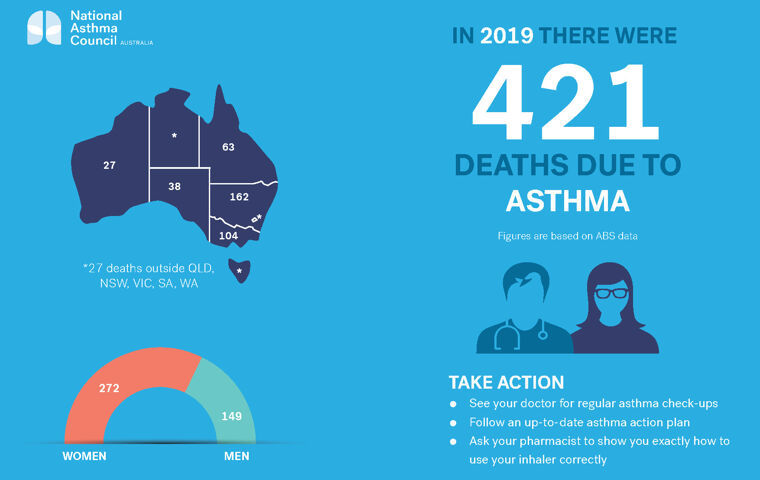
(Supplied by National Asthma Council)
Dr Burdon, however, understands that GPs often have limited consultation time and said, depending on the practice set up, trained practice nurses could assist with patient education and checking inhaler technique.
‘If you’re not using your inhaler properly, you might as well not be bothering with taking a treatment because the idea is to get what’s in the inhaler into the lung,’ he said.
‘If you’re using a metered dose inhaler, such as Ventolin, I always tell people, at least to start with, to stand in front of the mirror. If you see smoke coming out of your mouth, you’re not doing it correctly.
‘So inhaler technique does need to be checked on a regular or semi-regular basis.’
Currently in the midst of grass pollen season, which typically runs from 1 October to 31 December in Australia’s south-eastern states, Dr Burdon says GPs should be on high alert to prepare patients.
‘This is a high-risk season,’ he said.
‘We know from observation from the thunderstorm asthma epidemic in 2016 that there were a lot of people who presented that night with bad asthma who were on preventive medication, but weren’t taking it regularly.’
In addition to patients with asthma, RACGP Education Strategy Senior Advisor Dr Ronald McCoy said it is important GPs ensure patients who experience hay fever, particularly with symptoms of wheezing and breathlessness, are also on their radar.
‘Some people didn’t know they had asthma – it was the first time they had it,’ he told newsGP.
‘There were also some people who had hay fever and they get a little bit of shortness of breath and they just thought it was part of hay fever, but you don’t get respiratory symptoms with hay fever – that’s seasonal allergic rhinitis.
‘So at this time of year, you really need to check your patients, especially if they have hay fever, for asthma symptoms, and for your patients who have asthma, make sure that they’re controlled well.’
To ensure GPs and practices are prepared, the RACGP is offering a gpearning activity, Identifying and managing risk factors for thunderstorm asthma.
Developed in partnership with the National Asthma Council Australia and the Victorian Department of Health and Human Services, the activity is designed to help GPs to understand the phenomenon, identify and manage environmental and patient risk factors, and outline patient appropriate education.
‘Identifying and managing risk factors for thunderstorm asthma’ is worth two CPD points and can be accessed via the RACGP website.
Log in below to join the conversation.
preventive medicine thunderstorm asthma Victoria
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?