News
Hay fever or COVID? GPs on alert as spring brings allergies
Hay fever season is only weeks away, posing challenges for GPs when seeing patients with respiratory symptoms.
 The looming spring hay fever season is set to pose a new challenge for GPs and healthcare workers, as pollen from ryegrass, ragweed and Paterson’s Curse fills the air and sets off allergic reactions.
The looming spring hay fever season is set to pose a new challenge for GPs and healthcare workers, as pollen from ryegrass, ragweed and Paterson’s Curse fills the air and sets off allergic reactions.
UPDATED
You wake up with a runny nose, coughing and sneezing.
It could be COVID-19 – or it could be hay fever, particularly if you are living in Victoria, one of the world’s allergy hotspots.
The looming spring hay fever season is set to pose a new challenge for GPs and healthcare workers, as pollen from ryegrass, ragweed and Paterson’s Curse fills the air and sets off allergic reactions.
That means GPs will have to be on alert to differentiate those with hay fever from suspected COVID patients.
Around 18% of all Australians experience seasonal allergic rhinitis at some point in their lifetimes, representing around 4.6 million people.
Victorian Deputy Chief Health Officer Professor Allen Cheng told newsGP that people with a history of hay fever and asthma should ‘seek advice’ around optimising the management of their condition.
‘In addition to the public health impact on COVID-19, masks may also provide some benefit for those with allergic rhinitis and asthma,’ he said. ‘Clinical judgement should be applied to determining whether rhinorrhoea represents COVID-19 or allergic rhinitis.
‘Factors that would make allergic rhinitis more likely include a history of seasonal rhinitis in previous years at a similar time of year and concomitant itchy nose and eyes. Factors that would make COVID-19 more likely include other respiratory symptoms [such as] sore throat, cough and anosmia or systematic symptoms [such as] fever and myalgia.’
Geelong GP Dr Bernard Shiu told newsGP that peak hay fever season will likely coincide with the state’s gradual easing of lockdown restrictions in coming weeks.
‘People will be more out and about. Hay fever can give similar symptoms to early COVID,’ he said.
‘GPs will have more hay fever sufferers coming in, asking for tests.’
Dr Shiu has called on GPs in areas where hay fever is prevalent to be ready for the seasonal surge.
‘Do we have strategies to say this is definitely hay fever – or should we screen all potential hay fever patients for COVID?’ he said.
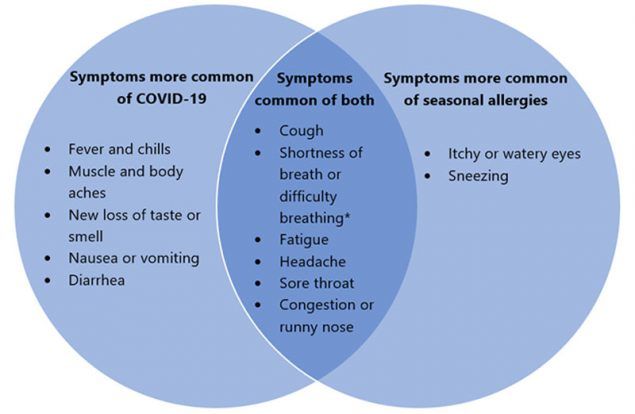
The US Centers for Disease Control and Prevention has produced a Venn diagram showing the overlap between hay fever and COVID-19. (Image: CDC)
Respiratory clinician and Asthma Australia adviser Dr John Blakey told the The Sydney Morning Herald the difference in symptoms between the new coronavirus and hay fever or asthma could be ‘difficult to untangle’.
Symptoms and timing are different depending on which part of Australia you live in, as Professor Janet Davies, head of the Allergy Research Group at Queensland University of Technology, told the ABC.
‘If you are looking at those places like Sydney, Canberra, Tasmania, Melbourne, Adelaide and even Perth, where we typically see a springtime grass pollen season peaking between October and the start of December, then because of the pollen season being short and sharp the hay fever that people get from pollen exposure tends to be quite acute,’ Professor Davies said.
‘Which means there will be a lot of sneezing associated with the hay fever, it will also be associated with itchy throat and itchy eyes.’
By contrast, Queensland’s grass pollen season usually runs much longer, from summer to autumn.
Victorian Chief Health Officer Brett Sutton has called on anyone with hay fever-like symptoms to get tested.
GP Dr Lara Roeske has backed these calls, telling the ABC it is important that anyone with respiratory symptoms who is uncertain as to whether it is hay fever should get a COVID test immediately.
‘In this environment, if you’ve got a runny nose for the first time, you’ve got a cough for the first time, a COVID test would be the first, most appropriate step rather than saying, “Let’s just take some antihistamines and see if this goes away”,’ she told the broadcaster.
‘People who regularly get hay fever will often know the symptoms well, such as the red, watery itchy eyes.
‘This is a common hay fever symptom, which you don’t get with COVID-19.’
Although the US Centers for Disease Control and Prevention does not link hay fever and anosmia, some people with hay fever can also experience reduced smell or taste, which may alarm them given anosmia is a tell-tale sign of COVID-19.
Log in below to join the conversation.
allergies COVID-19 hay fever
newsGP weekly poll
As a GP, do you use any resources or visit a healthcare professional to support your own mental health and wellbeing?