News
Ketamine effective for treatment-resistant depression: Study
New Australian-led research shows a 10-fold treatment advantage for the drug compared with placebo.
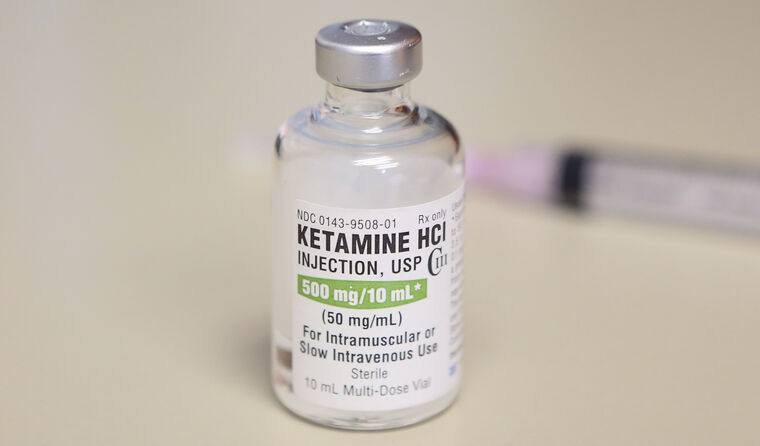 Treatment involved subcutaneous ketamine twice a week for four weeks, at a much smaller dose than what is generally used in a recreational setting. (Image: AAP)
Treatment involved subcutaneous ketamine twice a week for four weeks, at a much smaller dose than what is generally used in a recreational setting. (Image: AAP)
Newly published results from a randomised controlled trial indicate that generic, low-cost ketamine is more effective than placebo in treating patients with treatment-resistant depression.
The study, published in the British Journal of Psychiatry, involved seven mood disorder centres across Australia and New Zealand and included 184 participants with treatment-resistant depression, defined as clinical depression that has not responded to two or more therapies.
It included patients with severe illness, with one quarter of participants previously receiving treatment with electroconvulsive therapy and failing to respond.
Lead researcher Colleen Loo, Professor of Psychiatry at UNSW and the Black Dog Institute, told reporters at a briefing to coincide with the publication of the research that the results are promising.
‘There was a 10-fold treatment advantage for ketamine treatment compared with placebo medication,’ she said. ‘This corresponds to a 20% remission rate for the treatment group, versus only 2% for the placebo group.’
Those in the treatment group were given subcutaneous ketamine twice a week for four weeks, at a much smaller dose than what is generally used in a recreational setting. The placebo group received a psychoactive control, in this case midazolam, and depression scores were assessed at the end of the four-week treatment trial.
Professor Loo explained that despite most patients not being formally classified as ‘in remission’ during the trial, many patients still experienced clinical benefits with a significant reduction in depressive symptoms.
Co-researcher Professor Paul Glue from the University of Otago in New Zealand said the results were in keeping with his own experience.
‘I’d say that of the people we’ve had through our clinic, and this is probably consistent with other centres internationally, somewhere between two thirds and three quarters of people have either a good or a complete response,’ he said.
Many other trials that have assessed ketamine in the treatment of depression have used a patented formulation that is administered intranasally and is reportedly up to 40 times more expensive.
This trial used a generic form of ketamine, which is currently listed by the Therapeutic Goods Administration (TGA) for use in anaesthesia and sedation, meaning that it is low cost and relatively easy to access. The researchers also simplified the administration process.
‘Generic ketamine up to now has been mainly given as an infusion into the vein that goes over anything from half an hour to four hours,’ Professor Loo said.
‘This requires quite a complex medical setup as well as careful medical monitoring. It makes the whole procedure more complex and also more expensive.
‘We gave ketamine by a simple injection using a small needle under the skin. This is a similar technique to how people might give themselves insulin who are diabetic.’
Professor Loo also described the rapid response that patients experience, but reiterated the importance of close monitoring in case the treatment was ineffective.
‘It can lift mood incredibly quickly,’ she said. ‘You can go from being severely depressed to completely well in one day.
‘But you can also go the other way in one day and then that’s not just depression but also suicidality.
‘It has to be very carefully managed and monitored.’
Due to the side effects, such as blood pressure changes and feeling drowsy or dissociating, Professor Glue said subcutaneous ketamine administration is limited to specialised clinics where patients can be monitored.
Despite no participants reporting cravings for ketamine during the trial, Professor Glue said the researchers were also wary about the potential for drug dependency.
‘Ketamine is used as a party drug, it does have abuse potential,’ he said.
‘One of the things we were very careful to watch out for was whether participants might become addicted to ketamine during the study.’
He also stated that there may be potential for oral use and self-administration at home as more is learnt about the drug, dosage requirements and side effects; however, more research is needed before this is considered.
Professor Anthony Rodgers, public health and clinical trials expert from The George Institute, who also worked on the study, said research into ketamine for severe depression was a long time coming and that we are entering a ‘new world’ for treatment-resistant psychiatric illness.
‘It has a fascinating history,’ he said.
‘It’s now more than 20 years since the first studies, sort of by chance, showed that there was a possibility of these transformative benefits of ketamine in severe depression.
‘It is an extraordinary time. I mean 10 years ago people might have said there’s very little new treatments in severe depression, and now there are dozens.’
The new research was published two weeks after the TGA approved psilocybin, the psychoactive component in magic mushrooms, for use in psychedelic-assisted psychotherapy for treatment-resistant depression, which the researchers say generated a lot of interest but doesn’t have the same level of evidence as ketamine.
Unlike psilocybin, ketamine treatment does not have to be prescribed in conjunction with extended psychotherapy sessions that can last up to eight hours.
‘We have literally about 10 times as much data on the use of ketamine in treatment-resistant depression, then we have for say psilocybin for treatment-resistant depression,’ Professor Loo said.
The Black Dog Institute currently runs a novel medication clinic for patients with treatment-resistant depression and provides a training program for psychiatrists who are interested in prescribing ketamine.
Log in below to join the conversation.
depression ketamine mental health psychedelics
newsGP weekly poll
How often do patients ask you about weight-loss medications such as semaglutide or tirzepatide?