News
‘Life-saving’ program must continue despite coronavirus
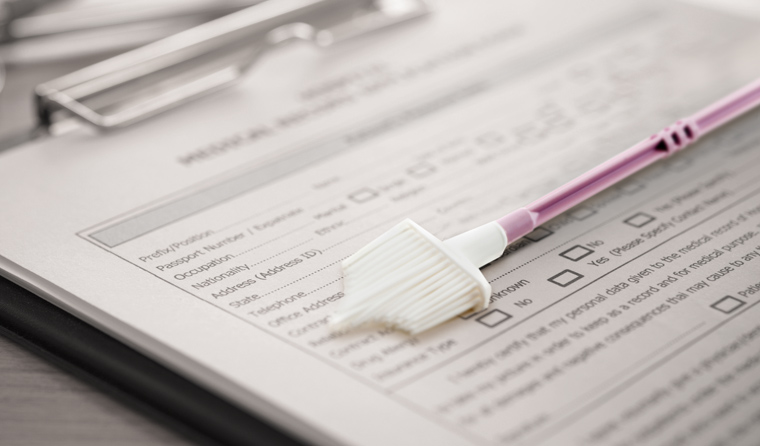
New guidance reinforces the importance of routine cervical screening and follow-up, but also offer options for when that’s not possible.
 The DoH resource presents a number of options to assist clinician decision-making, depending on individual patient circumstances.
The DoH resource presents a number of options to assist clinician decision-making, depending on individual patient circumstances.
According to the new resource, the Department of Health (DoH) has received ‘a number of enquiries’ from healthcare providers related to the program and how they can best support patients during the coronavirus pandemic.
While acknowledging some patients may feel ‘uncomfortable or worried’ about presenting for screening, the DoH stresses it is ‘important’ to offer and encourage routine screening and follow up wherever possible.
Co-author and working party member of the National Cervical Screening Program (NCSP) guidelines Dr Lara Roeske told newsGP the prevention of cervical cancer remains one of the ‘core’ services GPs provide and that this work must continue, even in the midst of a pandemic.
‘It is incredibly important that we consider the health of women, and in particular the services that we provide around sexual and reproductive health so that women don’t miss out – especially vulnerable groups of women,’ she said.
‘Screening is a life-saving measure and has worked very effectively in this country to reduce both this disease and deaths from cervical cancer.’
Dr Roeske also said GPs should be alert to patient apprehension and ensure appropriate outreach, in order to help facilitate an informed discussion regarding their options.
‘Patients that are currently participating in the program do require support and information, which could occur over a telephone call or video conference, around options in terms of accessing appropriate follow up – particularly for abnormal cervical screening results,’ she said.
‘Women should then be supported to make an informed decision about coming in to the practice.
‘For follow up of abnormal screening results there is no evidence available to inform us about what might happen to any one woman during a window period or delay period of 3–6 months. So the program would not support that and GPs would need to have a clear discussion about any potential deferment and the need for timely follow-up testing.
‘The ideal time to bring a woman in is when she’s due, or soon after, rather than earlier or much later.’
For this reason, Dr Roeske said it is important for GPs to remain alert to higher-risk patients within the pathway.
‘GPs should consider and it would be most appropriate to discuss a patient’s specific circumstances with a referring specialist or public colposcopy clinic to ensure timely access to investigation and treatment,’ she said.
‘This is particularly relevant for patients who may be at an elevated risk and require timely access to colposcopy – women aged over 50 years, Aboriginal and Torres Strait Islander women, or women who are immune deficient.
‘It continues to be necessary for women to come in to see their GP, so that they can have an appropriate internal examination to obtain a cervical sample as part of screening, or follow up of a previously abnormal cervical screening test result.’
However, with some clinics’ capacities and arrangements for managing patients also affected, apprehension about coronavirus may not be the only obstacle to maintaining routine healthcare.
To help GPs manage this uncertainty, the DoH resource presents a number of scenarios and options to assist clinician decision-making, including for deferral and rescheduling, depending on individual patient circumstances.
‘If women prefer not to attend in person, then rescheduling appointments for follow up in 3–6 months’ time may be considered for routine cervical re-screening for women with a previously negative screening history who are otherwise well, or for women who turn 25 and are yet to commence screening,’ Dr Roeske said.
‘For symptomatic women, under-screened or never-screened women, and women in the Test of Cure pathway, deferral or rescheduling is not recommended and these patients should be offered an appointment without delay.’
The temporary suspension of some non-urgent elective surgery has also impacted the treatment pathway and GPs must take this into consideration, Dr Roeske said.
According to the Royal Australian and New Zealand College of Gynaecologists (RANZCOG), colposcopy-associated treatment is considered a category 2 elective surgery (with suspicion of invasion category or glandular pre-cancer [ACIS] category 1).
All women with proven CIN2+ are considered either Category 2 (urgent) or Category 1, while patients with confirmed lesions of CIN2+ should also be treated with urgency.
Diagnostic colposcopies for women with any higher risk HPV and possible high-grade cytology or worse (pHSIL+), or suspicion of cancer, should be prioritised as urgent referrals.
Dr Roeske added that while the routine use of gloves at the time of cervical sampling is standard, the use of other personal protective equipment will vary for different practices and according to availability, patient request, individual clinical circumstances and GP preference.
‘Overall the risk of COVID-19 transmission in general practice remains low,’ she said.
‘However, the use of surgical masks, protective eyewear and a gown for intimate clinical examination and cervical sampling may be considered.’
Cervical screening advice for GPs
The following groups of women should be offered timely access to an in-person screening or follow-up appointment without delay:
- two or more years since the last Pap test – offer a CST at the time of presentation
- over 30 years of age and never screened – offer a CST without delay
- possible symptoms of cervical cancer (all post-menopausal bleeding, unexplained or abnormal post-coital or inter-menstrual bleeding, unexplained blood stained persistent vaginal discharge or persistent deep dyspareunia) require a clinical examination of the cervix, a co-test and referral for gynaecological assessment
- higher risk screening results – arrange a referral to a specialist for further investigation without delay
- in follow up on the Test of Cure pathway – should be seen on time for a co-test at least 12 months after treatment and annually until two negative co-tests
Groups of women in which a delay of 3–6 months may be considered include:
- women who turn 25 this year and are eligible to commence screening, as this group has substantial protection against HPV types either through direct HPV vaccination at school or indirectly via herd immunity. Therefore re-scheduling of screening appointments for 3–6 months for this group is considered low risk
- women currently in the intermediate risk pathway in 12-month follow up for a non 16/18 HPV positive and negative/low grade cytology screening result should ideally be seen at 12 months; however, a delay of 3–6 months is acceptable
Self-collection* should be considered for:
- all women over 30 years of age who have never been screened or are under-screened (more than four years since the last Pap test), and refuse a speculum exam
- women who have had a HPV non 16/18 positive result on a self-sample can access self-collection for the 12-month follow up HPV test
*There is currently a shortage of swabs that can be used for both self-collection and COVID-19 testing, so GPs are encouraged to use discretion when offering self-collection by proactively supporting the aforementioned categories of women.
Log in below to join the conversation.
cervical cancer cervical screening coronavirus COVID-19 HPV
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?