News
GPs have greater confidence in renewed cervical screening program
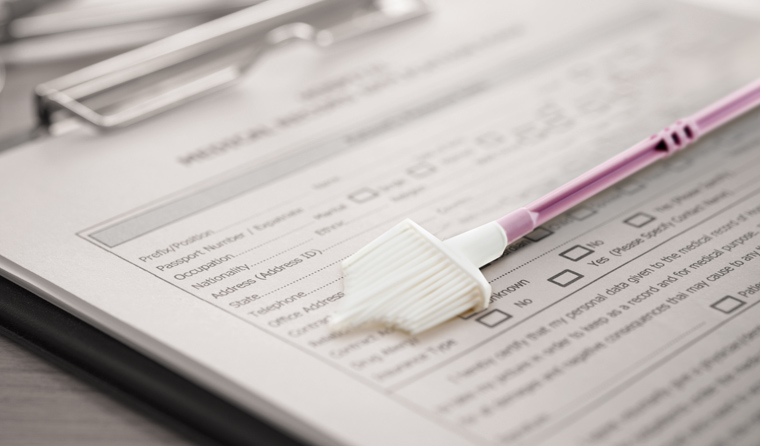
But the self-collection pathway remains an area of uncertainty, according to new research.
 Researchers found that a higher proportion of practitioners in the post-renewal period were more comfortable offering routine screening to women aged 25 or older.
Researchers found that a higher proportion of practitioners in the post-renewal period were more comfortable offering routine screening to women aged 25 or older.
Australian GPs have increased confidence and feelings of preparedness in implementing the National Cervical Screening Program since it underwent major changes in December 2017.
That is what new research published in PLOS one has found.
The research comprised two surveys of cervical screening providers in primary care. Its aim was to assess the level of preparedness of such providers in undertaking cervical screening before (pre-renewal, in 2017) and after (post-renewal, in 2018) the new program was implemented.
A total of 395 surveys were returned.
The researchers found that a higher proportion of practitioners in the post-renewal period were more comfortable offering routine screening to women aged 25 or older, and more confident explaining the rationale for not screening women younger than 25.
Furthermore, a higher proportion of practitioners in the post-renewal period were also more confident explaining a positive human papillomavirus (HPV) 16/18 and HPV non 16/18 test result.
Providers were also more comfortable not referring women with a positive HPV non 16/18 test result and low grade/negative cytology for colposcopy.
Study co-author Associate Professor Julia Brotherton is a public health physician at the VCS Foundation (formerly known as the Victorian Cytology Service).
She told newsGP that while these results will come ‘as little surprise’ to GPs, the survey uncovered other, more concerning results.
‘The most disappointing – but I guess not surprising thing, really – is that the area of least confidence remains self-collection,’ Associate Professor Brotherton said.
‘As we know, the self-collection pathway is restricted at the moment to under-screened and never- screened women.’
Associate Professor Brotherton said an ongoing problem revealed in the research is limited understanding of this pathway.
‘[Providers are] still lacking confidence in that pathway in exactly how to implement it,’ she said.
Associate Professor Brotherton said it is also vital to continue explaining to patients how effective the self-collection pathway is.
‘I think it’s really important to understand that, since the renewed program was designed, we actually have more data supporting the use of self-collection,’ she said.
‘In fact, we now know it is just as sensitive as a clinician-collected test for HPV, so we can actually have robust confidence in recommending this as a screening pathway for women who are under- and never-screened.
‘And, in fact, in the future I’m going to predict we’re going to see this as a mainstream option for cervical screening.
‘We’re not there yet, but if you’re speaking to a woman who’s considering the self-collection pathway you can certainly tell her, with confidence, that her test is going to be just as good as if you had taken it yourself.
‘That’s a really important message; that women shouldn’t be thinking that they’re getting an inferior test if they choose that pathway.’

Associate Professor Julia Brotherton believes it is important for patients to develop more confidence in the self-collection pathway.
The other key message Associate Professor Brotherton would like to convey relates to explaining the program’s test results to patients.
‘Unfortunately, some women are still confused [about test results],’ she said.
‘And I think it’s really important to take the time when feeding those results back, remembering that not all women are familiar with the idea that HPV can cause these lesions and cervical cancer, but most of the time it doesn’t.
‘So it’s really important when you’ve got a woman with an HPV-positive result, explaining this to her, explaining this is a risk-based program. It certainly doesn’t mean she’s got cancer.’
Associate Professor Brotherton said the way test results are conveyed to patients is imperative, as it has further implications.
‘The way we explain [results] is really going to support them in attending to the follow-up pathway appropriately and making sure everybody has the best outcome with the least anxiety,’ she said.
On 1 December 2017, Australia’s national cervical screening program changed from a two-yearly Pap test for women aged 18–69, to a five-yearly HPV test for women aged 2574.
Further changes included differential management pathways for oncogenic HPV 16/18 positive, versus HPV non 16/18 positive test results, as well as an option for self-collection of under-screened women.
Log in below to join the conversation.
cervical cancer cervical screening test HPV
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?