News
Mixed response to latest Solidarity trial COVID findings
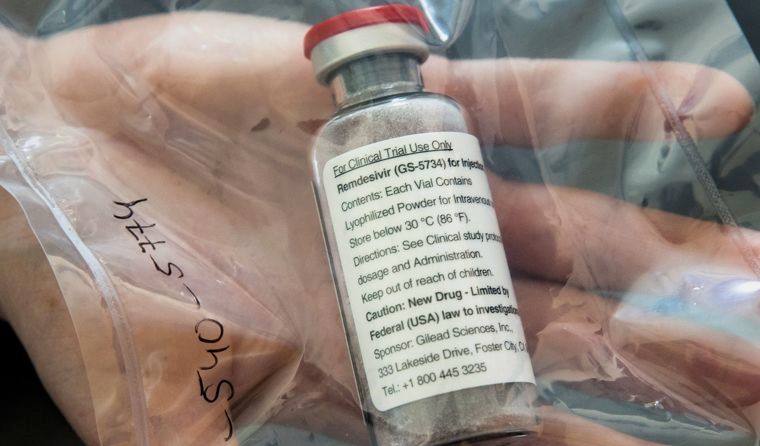
No therapeutics in the trial – including remdesivir – were found to affect on mortality or illness duration, but some say there is hope.
 While the results were disappointing, some experts say more detailed research is required. (Image: AAP)
While the results were disappointing, some experts say more detailed research is required. (Image: AAP)
Pre-print interim results from Solidarity, the world’s largest randomised control trial on COVID-19 therapeutics, indicate that remdesivir, hydroxychloroquine, lopinavir/ritonavir and interferon regimens have little or no effect on 28-day mortality or the in-hospital course of COVID-19 among hospitalised patients.
While the benefits of hydroxychloroquine have long been disputed, the repurposed therapeutics have all been promoted as potential existing treatments that could be used on COVID patients immediately, and remdesivir has been approved for use in Australia for several months.
Royal Melbourne Hospital infectious diseases clinician and co-lead of clinical research at the Doherty Institute, Associate Professor Steven Tong, told newsGP the results are disappointing, although in the case of remdesivir, are unlikely to affect his clinical behaviour.
‘I want to see treatments that work for COVID. So there’s a sense of disappointment that they didn’t find anything that worked across the four different therapies that they tried,’ he said. ‘[But] all the other [remdesivir] trials to date have not shown a mortality benefit, so this in reality probably accords with that.
‘Our current practice is based on the Australian National Medicine Stockpile criteria. That’s the only way we can access remdesivir anyway, and that is principally for patients who are on supplemental oxygen.
‘In that group there’s probably going to be still benefit in terms of getting them out of hospital earlier.
‘The ACTT-1 trial showed that the time to clinical improvement was reduced if you got remdesivir, and if there’s any group that’s going to have some mortality benefit, it’s going to be that group.’
Associate Professor Tong also pointed out that the ‘pragmatic’ nature of the Solidarity trial meant it could only capture a limited number of data points, and that it had not tracked when medication was given to patients.
‘They’ve recorded whether the patient is ventilated or not ventilated, and also the number of days from hospitalisation, but I don’t think they collected a number of days from symptom onset,’ he said.
‘It may well be that remdesivir might work better if it’s [taken] within five days of your symptom onset, but not if it’s after that – but we don’t know from the data they provide.
‘Solidarity continues, it’s not a finished or completed trial. So they may well be continuing to randomise within, for example, that supplemental oxygen group to receive remdesivir or not … [and] those confidence intervals that we’re seeing, may well narrow further as they get more patients.
‘We’re getting more and more of a picture that the use of antivirals earlier is better.’
Solidarity, which is coordinated by the World Health Organization (WHO) and spans more than 500 hospital sites across 30 countries, looked at the effects of these treatments on overall mortality, initiation of ventilation, and duration of hospital stay in hospitalised patients.
As a result, the researchers said other uses of the drugs, such as for treating patients in the community or for prevention, need to be examined using different trials.
A number of Australian researchers, including La Trobe epidemiologist Associate Professor Hassan Vally and public health academic and vaccine developer Professor Nikolai Petrovsky, said the results were not especially surprising and indicate a need to focus efforts on other potential treatments.
However, the Director of the Centre for Innate Immunity and Infectious Diseases Professor Paul Hertzog said he ‘would urge caution before abandoning’ research into interferon regimens due to the design of the trial.
‘Firstly, the route of administration might not be ideal. The interferon β1a was mostly delivered subcutaneously, which is not the best way to deliver interferon β1a to the lungs and is known to be less efficient than intravenous or inhaled. The latter is being trialled,’ he said.
‘Secondly, about half of the patients received corticosteroids at the same time and these are known to block interferon responses.
‘Thirdly, recent papers have indicated that certain patients might not be responsive to interferon since they produce antibodies to interferon or have mutations in interferon response pathways.
‘Fourth, interferon β1a may not be the ideal type to use [there are 20 different ones with different characteristics].’
Professor Hertzog also said the stage of disease affects the efficacy of an interferon’s antiviral properties.
‘The earlier it is given, the better chance it has of limiting damage from the virus,’ he said.
‘In the natural course of infection, several types of interferon out of the available repertoire of 20 different types are produced rapidly to limit local infection.
‘Strategic identification of the patients to treat, their concurrent medications, the type of interferon to use and its mode and timing of delivery may yet see these premier antiviral cytokines be used to good effect in the multipronged approach to treating infection with SARS-CoV-2.’
Professor Eleanor Fish from the Department of Immunology at the University of Toronto offered a similar warning.
‘I have several reservations about the trial design. Notably, at entry into the trial some patients required oxygen and others mechanical ventilation. Certainly for those that received interferon-beta, only 10 of the 482 cases did not requires any oxygen at entry into the trial,’ she said.
‘Given that all the emerging evidence points to interferon treatment being effective at the early, viral phase of COVID-19, treatment when patients are in the pulmonary or hyper inflammatory phases of COVID-19, ie later in disease, would likely be ineffective.
‘Close scrutiny of the data in the MedRxiv preprint shows that the 10 cases that received interferon-beta and who did not require supplemental oxygen did exhibit a significantly improved outcome in the context of mortality, compared with the 13 who also did not require oxygen and were not treated with interferon.
‘Until such time as all the data are scrutinised to evaluate the different subgroups of patients, their phase of disease and their rate of viral clearance, it is premature to dismiss some of these repurposed drugs as “ineffective” and to suggest they should not be evaluated further.’
According to the WHO, newer antiviral drugs, immunomodulators and anti-SARS CoV-2 monoclonal antibodies are now being considered for further evaluation in the Solidarity trial.
Log in below to join the conversation.
COVID-19 remdesivir Solidarity trial
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?