News
Antiviral becomes first recommended treatment for COVID-19
newsGP speaks with the Chair of Australia’s National COVID-19 Clinical Evidence Taskforce about the recommended use of remdesivir.
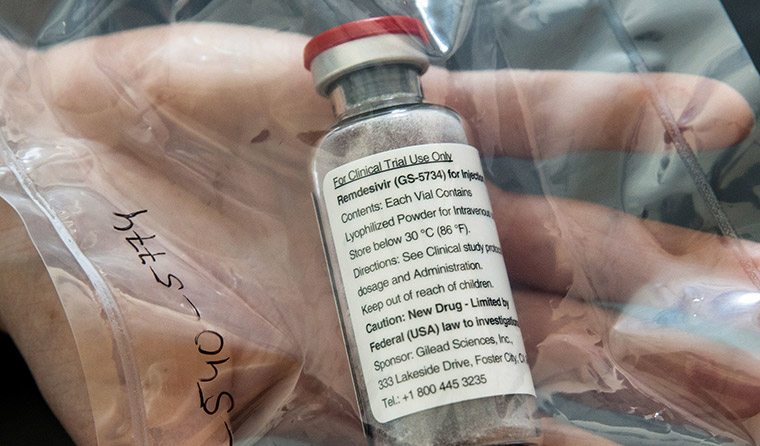 It is recommendation clinicians use the antiviral to treat adults who have been hospitalised with moderate, severe or critical COVID-19. (Image: AAP)
It is recommendation clinicians use the antiviral to treat adults who have been hospitalised with moderate, severe or critical COVID-19. (Image: AAP)
In what has been hailed as a ‘significant step forward’ by Associate Professor Julian Elliott, Chair of Australia’s National COVID-19 Clinical Evidence Taskforce (the taskforce), remdesivir has become the first medication recommended in Australia as a considered treatment for COVID to aid recovery time.
In its latest update, the taskforce made a conditional recommendation for clinicians caring for coronavirus patients to consider using the antiviral to treat adults who have been hospitalised with moderate, severe or critical COVID-19.
‘This is the first time we’re able to recommend a treatment for COVID-19,’ Associate Professor Elliott told newsGP.
‘From the preliminary data published so far, we can definitely say we have confidence that remdesivir reduces the time to recovery.’
The recommendation is based on preliminary data from two randomised controlled trials that have been published on the drug – a clinical trial in China published in The Lancet on 29 April, and a preliminary report from the Adaptive COVID-19 Treatment (ACTT) trial in the US published in The New England Journal of Medicine on 22 May.
More data is expected to come following the completion of the ACTT trial.
‘As of today, we can’t say if it has any effect on mortality,’ Associate Professor Elliott said. ‘But I think for people who are still seriously unwell, who are hospitalised, as we recommend, it should definitely be considered as a potential treatment.’
Originally developed to treat ebola, on 1 May remdesivir became the first therapy for COVID-19 to receive approval by the US Food and Drug Administration for emergency use.
While the drug is not currently licensed for use in Australia, the Federal Government has approved exemptions to some aspects of the Therapeutic Goods Act, granting access to remdesivir in the context of clinical trials and for compassionate use.
‘What we know is that there was an initial expanded access program that was established by the manufacturer at five hospitals. We understand that that is now being increased, and that the [Australian] Government is in discussion with the manufacturer about that,’ Associate Professor Elliott said.
‘The indication we’ve had from the Government is that they feel confident that the supply is sufficient at present.’
The recommendation is conditional, suggesting that use of the drug be a process of shared decision-making.
‘Doctors, other healthcare professionals, together with the patient, their family and carers, need to look at what we know so far on benefits and potential risks, and then make a decision together about whether to initiate treatment,’ Associate Professor Elliott said.
There are 10 clinical trials for remdesivir currently registered, and they are expected to recruit more than 14,000 patients in total.
While the current recommendation is only for adult patients who have been hospitalised, Associate Professor Elliott believes emerging data could hold promise for primary care.
‘The recommendation at the moment is not for patients with mild disease, but in the future we may have data, and we would hope to be able to determine whether remdesivir is also effective for people with milder illness,’ he said.
Established in April, the taskforce has been extensively reviewing and updating emerging COVID-19 research. Understanding the need for the latest clinical guidance, it took expert panels just under two weeks to review the latest evidence on remdesivir.
The new recommendation comes days after reports emerged calling into question the validity of data used for a Lancet study, which led the World Health Organization to pause the hydroxychloroquine arm of its global Solidarity Trial.
Australian researchers were among those who actively contributed to identifying the discrepancies, helping to push the process of investigation forward.
‘It’s breathtaking, really,’ Associate Professor Elliott said.
‘The taskforce has reviewed that paper, and prior to the retraction was aware of the controversy and had decided not to change its recommendation that hydroxychloroquine should only be used in the context of a clinical trial. So that recommendation will remain until we get further data.’
Given the serious implications that could result from unreliable data, particularly in a pandemic environment, Associate Professor Elliott said the taskforce is highly conscious of maintaining quality processes.
‘Traditionally, people who used evidence and guidelines have had a terrible choice, because you tend to have this tradeoff between really rigorous, high-quality approaches to synthesising research and reducing guidelines, or moving quickly,’ he said. ‘Previously it hasn’t been possible to do both at the same time.
‘That’s at the heart of what the taskforce is doing, using all of the rigorous processes that have been developed in evidence-based medicine over the last 30 years. But we’re just using novel processes and technologies to be able to do it much faster.’
Log in below to join the conversation.
coronavirus COVID-19 remdesivir
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?