News
Monkeypox now a disease of ‘national significance’
The declaration was made by Australia’s CMO, while ATAGI has also released updated guidance on vaccination.
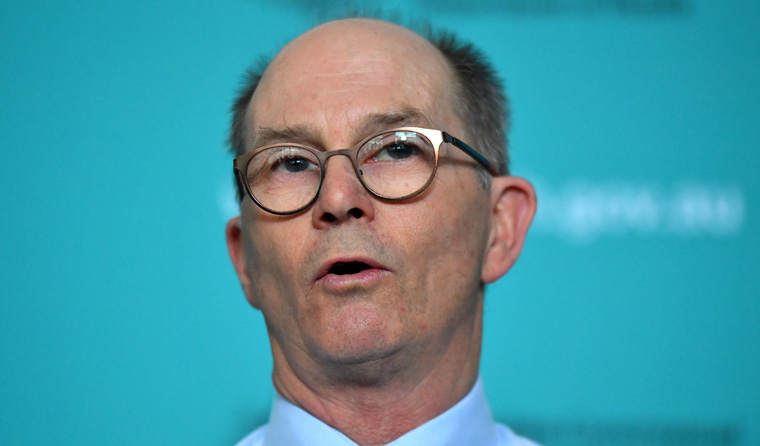 Australia’s Chief Medical Officer Professor Paul Kelly has declared monkeypox a Communicable Disease Incident of National Significance. (Image: AAP)
Australia’s Chief Medical Officer Professor Paul Kelly has declared monkeypox a Communicable Disease Incident of National Significance. (Image: AAP)
The ‘unfolding situation’ regarding monkeypox in Australia has been declared a Communicable Disease Incident of National Significance by Chief Medical Officer Professor Paul Kelly.
The announcement follows a World Health Organization (WHO) decision from 23 July to declare a public health emergency of international concern, with it having spread to at least 20,311 people in 71 countries where the disease is not endemic.
However, while now an incident of national significance, Professor Kelly moved to ease concerns by reminding people that no one is known to have died as a result of the current outbreak, and that monkeypox is far less transmissible and harmful than COVID-19.
‘The decision … was made under the Emergency Response Plan for Communicable Disease Incidents of National Significance, in consultation with the Australian Health Protection Principal Committee,’ he said.
‘Since May … public health experts have engaged with at-risk communities in partnership with key stakeholders and have been working very closely with their counterparts in state and territory health departments to ensure our response to monkeypox has been swift and coordinated.
‘The National Incident Centre has been activated to provide enhanced national coordination to assist states and territories to effectively manage the outbreaks within their jurisdictions.’
So far in Australia there have been 44 cases – the majority of which have been found in returned international travellers. Most cases have been among gay, bisexual and other men who have sex with men aged 21–40 years.
Although monkeypox is not usually considered a sexually transmissible infection, Professor Kelly said sexual intercourse with an infected person carries a ‘significant risk of transmission’, as does intimate physical contact such as hugging and kissing, with infectious skin sores judged to the ‘likely mode of transmission’.
To date, monkeypox’s rash and flu-like symptoms have been relatively mild, and in most cases, resolved within 2–4 weeks without the need for specific treatments.
The rash can vary from person to person and take on the appearance of pimples, blisters or sores. In this outbreak it is being seen especially on the genital and perianal regions of affected people, but it also usually occurs on the face before spreading to other parts of the body, including the palms of the hands and the soles of the feet.
The flu-like symptoms often include fever, chills, body aches, headaches, swollen lymph nodes and tiredness.
While Professor Kelly notes that most cases do not require specific treatments, the National Medical Stockpile has made antivirals available to states and territories upon request.
Clinical guidance on vaccination
The Australian Technical Advisory Group on Immunisation (ATAGI) has updated clinical guidance on vaccination against monkeypox to include the use of the third generation MVA-BN vaccine to prepare for it being made available in Australia.
The Commonwealth and some states and territories have already secured limited supplies, and it is the preferred vaccine for both pre-exposure prophylaxis and post-exposure prophylaxis, due to its more favourable safety profile and comparative ease of administration.
ATAGI recommends the following key risk groups should be considered for vaccination:
- Anyone categorised by public health authorities as a high risk monkeypox contact in the past 14 days
- Gay, bisexual and other men who have sex with men, who are at the highest risk of monkeypox infection due to having a high number of sexual contacts. Risk criteria for infection may include:
- those living with HIV
- a recent history of multiple sexual partners, participating in group sex, or attending sex on premises venues
- other proxy markers, such as recent sexually transmitted infection or those being advised to take HIV PrEP due to number of sexual partners. While many people prescribed HIV PrEP are monogamous with a HIV positive partner, this category can also capture those with multiple partners who are at high risk
- those who have received a recommendation from other service providers, such as sexual health clinics.
- Sex workers, particularly those whose clients are in high-risk categories
- Immunisation providers who are administering the ACAM2000 smallpox vaccine, if they have not previously received a smallpox vaccine
Anyone in the above risk categories planning travel to a country experiencing a significant outbreak should also consider getting immunised, with vaccination ideally taking place 4–6 weeks prior to departure.
A booster dose is recommended for people in key risk groups who received a smallpox vaccine more than 10 years ago, with both available vaccines deemed suitable.
Further information about monkeypox is available on the
Department of Health and Aged Care website.
Log in below to join the conversation.
monkeypox vaccination
newsGP weekly poll
Sixty-day prescriptions have reportedly had a slower uptake than anticipated. What do you think is causing this?