News
DoH releases primary care guidelines for vaccine blood clots
The Department of Health document outlines possible presentations, symptoms and signs to look out for, as well as initial investigations.
 In Australia thrombosis with thrombocytopenia syndrome has commonly presented as deep vein thrombosis and pulmonary emboli.
In Australia thrombosis with thrombocytopenia syndrome has commonly presented as deep vein thrombosis and pulmonary emboli.
Correction: This article was updated at 8.00 pm on 14 July to confirm that the majority of TTS cases occur after the first dose of AstraZeneca, not the second as was previously reported.
As it stands, the incidence rate of developing thrombosis with thrombocytopenia syndrome (TTS) in Australia after receiving AstraZeneca’s COVID vaccine is 2.8 per 100,000 in those aged under 60, and 1.7 per 100,000 in older cohorts, with the majority of cases occurring after the first dose.
To date, 76 confirmed and probable cases have been reported in Australia out of more than five million doses of the vaccine, three of which have proved fatal.
But with understanding of the syndrome having developed over time, the Department of Health (DoH) has released new guidelines to assist GPs in recognising, responding to and managing suspected presentations.
When should GPs suspect TTS?
According to the guidelines, TTS (also known as vaccine-induced immune thrombotic thrombocytopenia [VITT]) should be considered in any patient who has received the AstraZeneca vaccine 4–42 days prior to presentation, and has signs or symptoms of either thrombosis or thrombocytopenia.
Possible presentations to look out for, include:
Cerebral venous sinus thrombosis (CVST)
- an unusual headache that starts or persists at least 48 hours after vaccination and is severe or does not improve following simple analgesia
- signs or symptoms of raised intracranial pressure, eg headache is worse when supine or associated with nausea and vomiting
- neurological deficit, eg blurred vision, dysarthria, altered mental status or seizures.
Thrombosis in the splanchnic (abdominal) circulation
- This is a variable presentation and can be asymptomatic
- Abdominal pain is the most common symptom, and accompanying symptoms may include gastrointestinal bleeding, nausea, vomiting, anorexia, fever, diarrhoea or constipation
Pulmonary emboli (PE)
- A sudden onset of chest pain and shortness of breath
Deep vein thrombosis (DVT)
- Lower limb pain, redness or swelling
Arterial thrombosis
- Signs or symptoms of arterial ischaemia include limb coldness or pallor
- Signs or symptoms of myocardial ischaemia or stroke
Thrombocytopenia
- Petechiae, purpura and acute onset bleeding, for example of the nose and/or gums
So far in Australia, TTS has presented more commonly as DVT and PE than CVST or splanchnic thrombosis, and patients may less commonly initially present with signs or symptoms of thrombocytopenia.
Next steps
If the patient is not acutely unwell and the practice can obtain and review the pathology results within six hours, the guidelines recommend GPs refer patients for initial investigations including:
- a full blood count, looking for thrombocytopenia (platelets < 150x109/L), while noting that the platelet count can initially be normal or fall from a higher baseline
- D-dimer: usually raised ≥5 times the upper limit of normal (ULN).
GPs are encouraged to repeat these investigations in 24–48 hours for patients whose results are ‘reassuring’ but have persistent symptoms, including those who have been discharged from the emergency department (ED) with reassuring results.
When is it time to refer to the ED?
According to the guidelines, in some suspected cases of TTS, an immediate referral to the ED may be more appropriate. This includes scenarios where blood tests cannot be performed and reviewed within six hours, and also if the patient:
- is acutely unwell, for example with acute neurological deficit, severe abdominal pain, severe bleeding or any other concerning signs or symptoms
- has thrombocytopenia or elevated D-dimer levels.
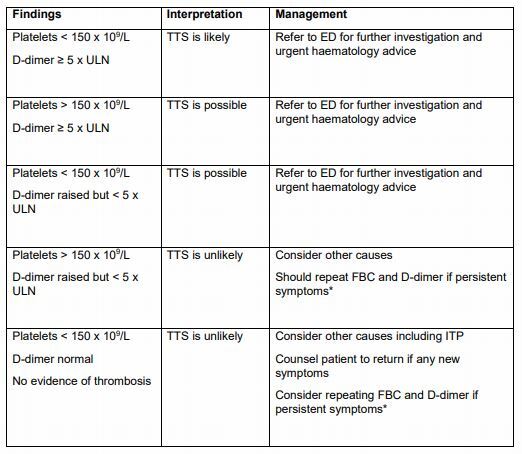 A table featured in the DoH’s guidelines, including interpretations and recommendations based on investigation results for patients with suspected TTS. (Image: Department of Health)
A table featured in the DoH’s guidelines, including interpretations and recommendations based on investigation results for patients with suspected TTS. (Image: Department of Health)
Up until now, GPs have been led by
guidelines released in May by the Thrombosis and Haemostasis Society of Australia and New Zealand (THANZ) VITT Communications Committee, which developed its own TTS guidelines.
NSW GP Dr Ai-Vee Chua contributed to the development of the THANZ Multidisciplinary guidelines for TTS and said while the DoH’s six-page document ‘spells things out quite nicely’, there are a few recommendations that deviate.
Where the Government-issued guidelines recommend full-blood count and D-dimer test results be obtained and reviewed within six hours and repeated within 24–48 hours for patients with normal results and persistent symptoms, the THANZ Multidisciplinary guidelines recommend that results be obtained and reviewed within four hours and repeated within a 24-hour period for patients with an elevated D-dimer normal platelet count and persistent symptoms.
In addition to full blood count and D-dimer testing, the THANZ Committee also recommends checking PT, APTT, and fibrinogen at the time of initial screening.
‘Our haematologists have indicated that there are two reasons for this,’ Dr Chua told
newsGP.
‘Firstly, low fibrinogen has been noted in some of the VITT cases – potentially the most severe ones. But also to exclude disseminated intravascular coagulation as a cause for low platelets and raised D-dimer.
‘The second reason for doing the full coagulation panel is that if there is a clot that is confirmed – whether it’s a VITT clot or a non-VITT clot – it is worthwhile having a baseline PT and APTT result prior to starting any form of anticoagulation.’
Another difference noted by Dr Chua is that there are more scenarios in which the DoH’s guidance recommends referral to an ED, whereas the THANZ guidelines have a greater emphasis on GPs using their individual clinical judgement.
‘It’s a special role we play as GPs; while guidelines exist, we must always ask how is this applicable to this particular patient sitting in front of me at this very point in time with the symptoms that they’re presenting with?’ she said.
‘We’ve got to bring that clinical judgment into play combined with our knowledge of our patients, and this includes considering whether they are best investigated initially in the community or in the emergency department and whether we need to consider other differential diagnoses beyond TTS.
‘If we had an automatic referral to emergency, I think that really makes it difficult for the integrated healthcare system as a whole. Our poor emergency departments would really find it difficult to be able to see those patients, as well as the normal care that they have to provide.’
Dr Chua said ultimately what GPs need is one uniform set of guidelines.
‘Ideally the Department of Health guidelines and the THANZ Multidisciplinary guidelines are each adjusted to ensure uniformity of recommendations. I think they could be worked to complement each other really well,’ she said.
‘At the moment there are some differences between the two that may well make it confusing for our doctors trying to look after a case of suspected VITT.’
Log in below to join the conversation.
AstraZeneca blood clots COVID-19 TTS vaccines VITT
newsGP weekly poll
Which of the following areas are you more likely to discuss during a routine consultation?