News
Over-screening of colorectal cancer putting patients at risk: Study
An abundance of ‘low-value’ colonoscopy services for bowel cancer screening is creating a bottleneck in which potentially at-risk patients are having their diagnosis delayed, new research has found.
 It has been found that more than 40% of colorectal cancers in Australia are diagnosed at stage three or stage four.
It has been found that more than 40% of colorectal cancers in Australia are diagnosed at stage three or stage four.
A new research paper, ‘Why don’t I need a colonoscopy? A novel approach to communicating risks and benefits of colorectal cancer screening’, published in the June issue of the Australian Journal of General Practice (AJGP) has explored the significant growth in demand for colonoscopies in Australia.
‘Over 700,000 colonoscopies were performed in Australia in 2012–13, with approximately 80% of these colonoscopies at least partially funded through the Medicare Benefits Schedule [MBS],’ co-author Professor Jon Emery told newsGP.
‘The MBS rebate for colonoscopies increased by 28% from 2012 to 2015.
‘It is alarming that so many Australian patients are undergoing unnecessary colonoscopies and potentially putting other patients at risk of delayed diagnosis.’
According to Professor Emery, diagnosis for colorectal cancer in Australia and New Zealand is often made in the later stage of the disease, despite the fact these countries have the rates of colorectal cancer in the world.
‘Currently, over 40% of colorectal cancers are diagnosed at Stage 3 or 4 in Australia,’ he said.
‘For every one million Australians aged 50 years and older, 80,000 people at average risk of colorectal cancer are being over-screened with colonoscopy, and 29,000 people at increased risk are not having the colonoscopy they need.’
Professor Emery and his research co-authors developed ‘expected frequency trees’ (EFTs) to demonstrate the projected outcome of Australians at average and moderate risk of colorectal screening options.
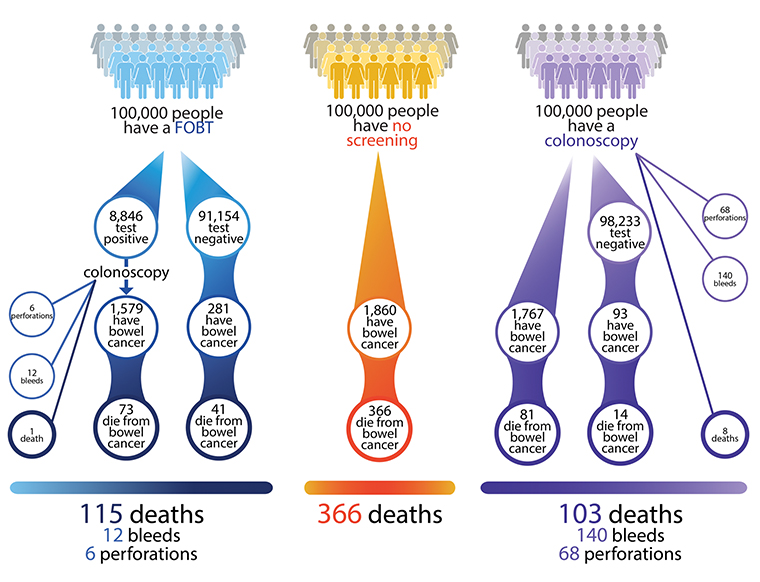
Expected frequency tree for population at moderately increased risk of colorectal cancer.
(Reproduced from Emery JD, Pirotta M, Macrae F, et al. ‘Why don’t I need a colonoscopy?’: A novel approach to communicating risks and benefits of colorectal cancer screening. Aust J Gen Pract 2018;47(6)343–49.)
‘These EFTs may challenge clinician and patient attitudes about the relative harms and benefits of two different screening methods for colorectal cancer,’ Professor Emery said.
‘Colonoscopic over-screening can be managed by GPs through correct referral pathways depending on the patient’s risk of colorectal cancer.’
Associate Professor Joel Rhee, GP and Chair of the RACGP Cancer and Palliative Care Specific Interests network, agrees that GPs are a vital part of the process of identifying patients at risk of colorectal cancer.
‘Colonoscopies should be reserved for patients at increased risk of bowel cancer, either because of their family history or because of symptoms which may be due to cancer,’ he told newsGP.
‘The National Bowel Cancer Screening Program will be an initial point of screening of asymptomatic patients aged between 50 and 74 who are in the average-risk category.
‘However, until 2020, when the program is scheduled to be fully implemented, patients aged between 50 and 74 should seek advice from their GP on whether they should get additional screening tests done.’
ajgp bowel-cancer-screening colonoscopy colorectal-cancer
newsGP weekly poll
How often do patients ask you about weight-loss medications such as semaglutide or tirzepatide?