News
RACGP 12-point opioid challenge
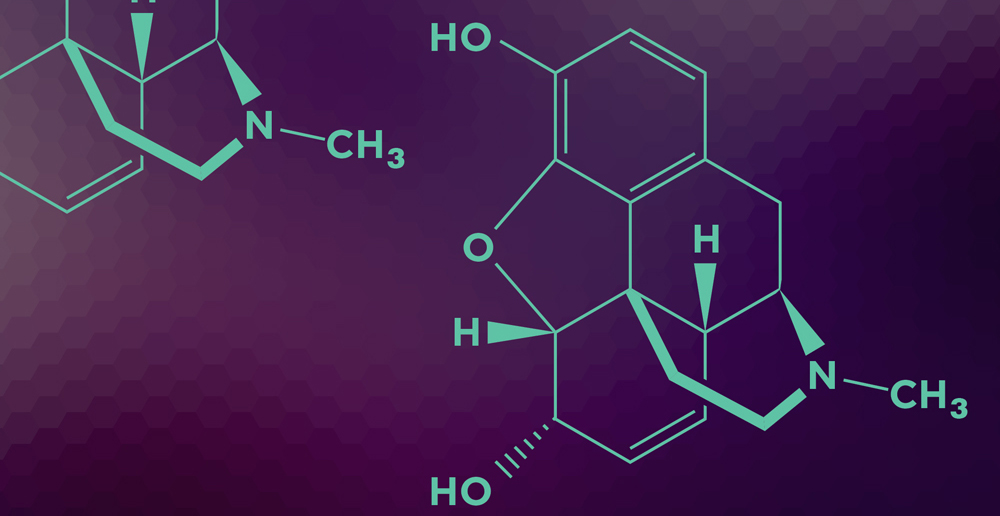
With the issue of pain management becoming increasingly prevalent in Australian healthcare, GPs are often at the forefront of dealing with patients experiencing chronic non-cancer pain. However, the role of opioids in treating these patients has raised increasing concerns about safety.
‘For many people, good pain management can transform their quality of life,’ RACGP President Dr Bastian Seidel said. ‘Unfortunately, what we have been seeing is an exploitation of painkilling medications.’
 Reducing opioid prescribing in general practice: 12-point challenge to GPs
Reducing opioid prescribing in general practice: 12-point challenge to GPs
Dr Evan Ackermann, lead author of the RACGP’s Prescribing drugs of dependence in general practice, has issued general practice with a 12-point challenge aimed at reducing opioid prescribing.
He encourages all GPs to undertake the challenge, which aligns with the recent launch of the latest part of Prescribing drugs of dependence in general practice – Part C1: Opioids and Part C2: The role of opioids in pain management.
Reducing opioid prescribing in general practice: 12-point challenge to GPs
For acute pain:
- Know when non-opioid analgesics are preferred for acute pain in general practice. For example, headache, dysmenorrhoea, dental pains, minor musculoskeletal strains/sprains.
- Engage a physiotherapist early in more severe acute musculoskeletal injuries.
- Prioritise non-opioid options for people who have been on long-term low-dose codeine preparations.
- If opioids are necessary for severe acute pain, limit prescription to three days’ supply.
- On discharge from hospital, discuss early tapering of opioids as part of recovery process.
For chronic non-cancer pain:
- Maximise non-opioid therapies and multidisciplinary care in chronic pain.
- Avoid opioids for chronic non-cancer pain in patients with an active or past substance-use disorder or unstable psychiatric disorder.
- Where opioid therapy is necessary, ascertain responsiveness below 50 mg morphine-equivalent dose per day and seek assistance well before 100 mg morphine-equivalent dose per day is reached.
- Reassess opioid-responsiveness regularly and often; have an agreed practice system for the 12-month structured review of opioid therapy.
- Undertake intermittent planned reductions of opioid dosage in chronic non-cancer pain management.
- Avoid fentanyl patches for non-cancer pain.
- Where existing patients are on >100 mg morphine-equivalent dose per day for chronic non-cancer pain, trial tapering this dose to more appropriate levels.
Join the pain management discussion led by Dr Ackermann in
shareGP.
opioids pain painkillers pain-management
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?