News
US purchasing global supply of COVID-19 drug raises ethical questions
Gilead Sciences has donated a supply of remdesivir to Australia’s national medical stockpile. But what if cases continue to rise?
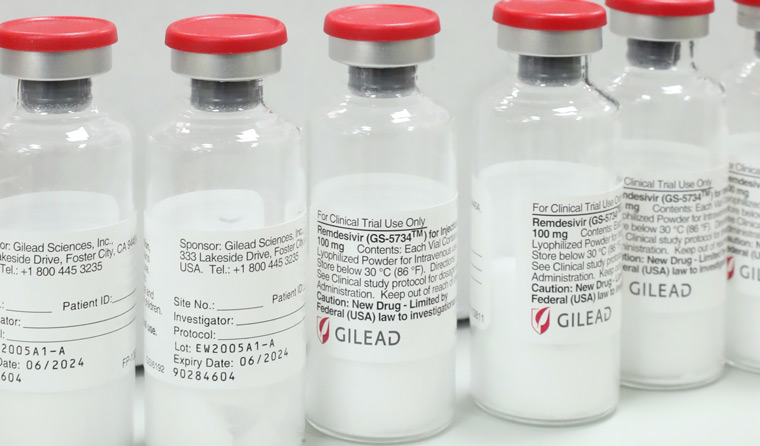 Gilead Sciences revealed treatment will cost US$390 per vial – US$2340 for a five-day course – a stark contrast to the estimated cost of production at less than US$1 per day. (AAP)
Gilead Sciences revealed treatment will cost US$390 per vial – US$2340 for a five-day course – a stark contrast to the estimated cost of production at less than US$1 per day. (AAP)
Federal Health Minister Greg Hunt has assured Australians that the Government has enough remdesivir to meet COVID-19 patient demand, despite reports of the US Department of Health and Human Services recently securing 500,000 additional courses of treatment.
The purchase represents 100% of Gilead’s production of the drug for July, and 90% of August and September, a move Associate Professor Julian Elliott, Chair of the National COVID-19 Clinical Evidence Taskforce, has branded ‘concerning’.
‘There’s obviously an issue here because the company only produces a certain amount of supply over the coming months,’ he told newsGP.
‘The question of how that’s distributed internationally is important because it’s certainly possible that around-the-world demand may outstrip supply.’
The antiviral, developed for use against Ebola, was the first drug to show promise as an effective treatment for patients hospitalised with COVID-19. While it has not been shown to reduce the mortality rate, preliminary data suggests remdesivir can cut recovery time by about four days.
Just over three weeks ago, Australia’s taskforce followed in the footsteps of the US and UK endorsing the use of remdesivir as a potential treatment for hospitalised patients with moderate to severe COVID-19.
In an open letter from CEO Daniel O’Day on 29 June, Gilead revealed that the treatment would cost US$390 per vial. Based on current treatment patterns, the vast majority of patients are expected to receive a five-day treatment course equating to US$2340 (AU$4607) for people in the US and other developed countries – a stark contrast to the estimated cost of production at less than US$1 per day or US$6 (AUD$ 8.64) for a six-day course of treatment.
The price tag has raised the ire of some, given the drug’s development was largely funded by taxpayers.
La Trobe University’s Dr Deborah Gleeson, a senior lecturer and researcher in trade policy and access to pharmaceuticals, said Gilead’s actions show that pharmaceutical companies cannot be ‘trusted to act ethically’ and that the current funding model for development needs a shakeup.
‘Governments need to attach conditions to their funding for research and development to ensure that drugs and vaccines for COVID-19 are shared equitably,’ Dr Gleeson said.
‘While a drug is under patent, companies can set high prices while keeping competitors out of the market. This presents obvious problems in a public health emergency, where rapid access to large supplies of affordable products is needed.
‘Gilead could make billions of dollars in profit during the pandemic, while preventing others from manufacturing the drug on the scale needed to meet global demand.’
Companies often try and justify the price tag as being necessary to recoup developmental costs of the drug, as well as others that did not make it to market.
‘The counter argument, of course, is from a public health point of view – it’s important to ensure that the pricing is aligned with the public health benefits and not a barrier to access, particularly in a time of a health crisis such as this,’ Associate Professor Elliott said.

Associate Professor Julian Elliott, Chair of Australia’s National COVID-19 Clinical Evidence Taskforce, has called the purchase of almost 100% of Gilead’s remdesivir production ‘concerning’.
A possible solution posed by Associate Professor Barbara Mintzes, from the University of Sydney’s Charles Perkins Centre and School of Pharmacy, is that governments, under international trade agreements in a public health emergency, can issue compulsory licenses to bypass patent protection and either produce a drug themselves or buy it from generic manufacturers.
The Netherlands is currently considering such a move for remdesivir.
‘Currently, we don’t know for sure whether remdesivir will prove to be an important treatment for COVID-19,’ Associate Professor Mintzes said.
‘If it does, given that the US is buying out Gilead’s supply, and also given the extremely high price as compared with costs of production, the obvious solution for Australia would be to also consider compulsory licensing.’
But as viral transmission in the US continues to climb – it recorded nearly 50,000 new cases on Wednesday 1 July in its biggest one-day spike to date – and pressure mounts on the US Government, Dr Roger Lord, a medical sciences lecturer at The Australian Catholic University, says the country’s decision is ‘not surprising’.
‘Australia is comparatively in a much better place in terms of controlling SARS-CoV-2 transmission and while remdesivir is under patent to Gilead, a pharmaceutical company does have both a moral and financial interest to increase production to meet demand,’ he said.
‘Once Gilead has secured the required legal and regulatory paperwork to allow for manufacture at other locations, the supply of remdesivir will become more widespread.’
Gilead currently has licensing agreements with manufacturers in Egypt, India and Pakistan to supply remdesivir to 127 low to middle-income countries at a lower price, but has yet to indicate by how much.
Beyond the antiviral, news of the US purchase has raised concern over a similar scene playing out with the development of a vaccine.
To ensure equitable access, Associate Professor Elliott says efforts are underway to avoid future hoarding of stockpiles, but admits the US’s unilateral action has the potential to ‘damage those attempts at a more collaborative international approach’.
The World Health Organization (WHO) recently warned that it is still early days in the pandemic, and that ‘the worst is yet to come’.
Victoria recorded 77 new coronavirus cases on Thursday 2 July, with 10 postcodes identified as hotspots returning to stage three lockdown as the testing blitz continues. One new case was confirmed in the Northern Territory – the first in 42 days – and eight in NSW up to 8.00 pm on Wednesday 1 July, among them a man who tested positive for COVID-19 while in hotel quarantine in Melbourne.
After returning to Sydney, the man worked while symptomatic for two days at Woolworths in Balmain before testing positive again. Fifty of his co-workers have been directed to self-isolate, and authorities have called on anyone in the area with even mild symptoms to get tested.
If Australia’s second peak advances rapidly, Associate Professor Elliott admits supplies of remdesivir would be cause for concern. But, as it stands, he says Australians ‘can feel reassured’.
‘Australia has got a very strong history of being able to negotiate well with companies,’ he said. ‘I don’t think there’s any reason for undue concern here at this moment.’
Log in below to join the conversation.
coronavirus COVID-19 remdesivir
newsGP weekly poll
How often do patients ask you about weight-loss medications such as semaglutide or tirzepatide?