News
Cervical screening self-collection to expand from July
Dr Lara Roeske outlines what GPs need to know about the ‘game-changing’ 1 July expansion.
 General practices can find out from their local laboratory whether they support self-collection.
General practices can find out from their local laboratory whether they support self-collection.
Cervical cancer is currently the 14th most common cancer in Australia, and in 2021 there were 913 new diagnoses and 237 deaths.
We know that about 72% of those diagnosed with invasive cervical cancer in Australia are under screened or never screened. And we know only about 52% of those people who are eligible participate in screening.
This means that as GPs, we all have patients in our practices that have either refused or are unable to take part in cervical screening in the conventional way – the clinician-collected way – for a whole range of reasons.
From 1 July, the expansion of self-collection to all people with a cervix under the National Cervical Screening Program (NCSP) means it will no longer be restricted to under-screened or never-screened women.
This landmark announcement made last year is a complete game-changer for cervical cancer screening.
Eligibility for self-collection
The self-collection option is available as part of the NCSP to all people with a cervix who are aged between 25–74 and who have ever been sexually active.
Aside from the outset when people who are asymptomatic are coming in to have routine screening, there are two points in the management pathways under the NCSP where self-collection can also be considered and offered:
- At the intermediate risk pathway at the 12- and 24-month follow-up human papillomavirus (HPV) testing mark
- After a total abdominal hysterectomy, provided it was for benign reasons with no evidence of cervical pathology and where there’s an unknown screening history
In addition, it is absolutely safe and appropriate to offer self-collection as a choice to women who are pregnant. It is also fine to self-collect during a period, we just suggest not during the heavy bleeding days.
Anyone requiring a co-test is not eligible for self-collection. Co-tests are required for five groups which include anyone:
- with symptoms suggestive of cervical cancer
- who is undergoing test of cure after treatment for a high-grade squamous intraepithelial lesion (HSIL)
- who has been treated for a glandular abnormality, including adenocarcinoma in situ (AIS)
- who has been exposed to diethylstilbestrol (DES) in utero
- who has had a total hysterectomy with a history of HSIL.
 Self-collection is an important tool for GPs, says Dr Lara Roeske, which helps give patients greater control around cervical screening.
The benefits of self-collection and GPs’ role
Self-collection is an important tool for GPs, says Dr Lara Roeske, which helps give patients greater control around cervical screening.
The benefits of self-collection and GPs’ role
It’s important that GPs are confident to explain the benefits of self-collection and encourage uptake of screening.
GPs are the major provider of cervical screening services Australia-wide, and the evidence has shown that they are very impactful around encouraging participation. But we have a way to go at a 52% participation rate, and with most cervical cancer occurring in under- and never-screened people, we really need to take up this option.
Our job going forward from 1 July is firstly to promote and educate patients around the self-collection option, and this has to be done as part of the consultation.
There is an expectation that GPs will still have a consultation with eligible people and that this can also be done via telehealth.
For many of us GPs who have been practising now for decades, we have been inserting a speculum and taking the sample directly from the cervix. So it’s a complete change in the way we practice but is a promoter of choice for participants in screening and we still have an absolutely critical role in this.
It’s a very important tool for the GP because it helps our patients to have choice and greater control around their experience with cervical screening.
There are particular groups that self-collection will be of benefit to, for example:
- people who have experienced sexual violence and trauma
- LGBTQI+ people
- Aboriginal and Torres Strait Islander people
- people from culturally and linguistically diverse (CALD) communities
- people living with disability.
In addition to overcoming cultural barriers, there is a big group of people who have had a negative experience with screening in the past, so they may experience fear or embarrassment around the process.
Self-collection really addresses many of those barriers and allows people control and dignity, and helps to remove that stigma.
A classic example is the 55-year-old, quite overweight patient who is post-menopausal. She’s declined a cervical screening test year-in, year-out. She feels embarrassed and says she’s not sexually active.
Or it’s the 28-year-old who has experienced sexual violence, is due for screening and would find a cervical screening very traumatising.
There are many of these examples in our practices and there may also be a group out there that don’t attend our practices.
Given that GPs work in a diversity of settings such as rural and remote areas, with refugee and asylum seeker groups, and Aboriginal and Torres Strait Islander people, we have oversight and responsibility around determining whether self-collection is the right option, and also around the follow up and management.
We can work closely with (for example) Aboriginal health workers, community health workers and CALD representatives to enable many – who otherwise would not – to actually access cervical screening.
GPs have a crucial role in determining together with the patient when self-collection is a good choice for them and then supporting them to take the test, as well as any follow up around results.
Discuss with patients what would happen with positive results or if HPV was detected and explain what the follow up and management would be in that case.
GPs also need to know the past cervical screening history of the patient they are offering screening to, to ensure that they make correct clinical decisions around management follow up.
The self-collection process
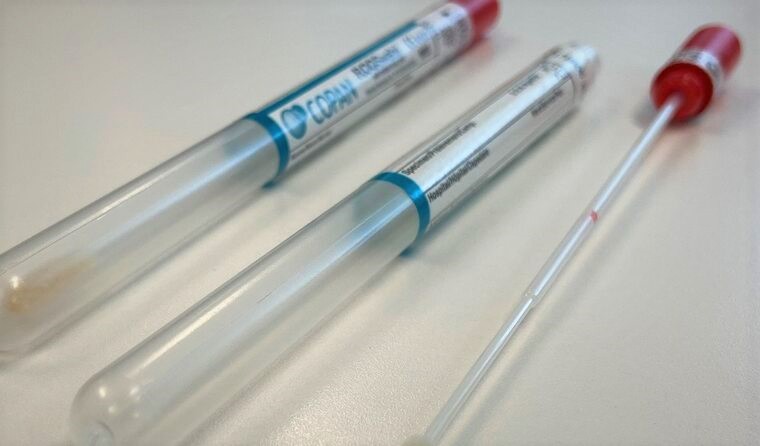
The
process of self-collection needs to be explained to patients in a sensitive and culturally appropriate way, highlighting that
it is as accurate an HPV test as a clinician-collected sample for HPV testing.
Australian research has confirmed that it is highly acceptable to people. We don’t want GPs to be concerned around either accuracy or acceptability.
When supporting patients to take the sample, GPs can orientate them to the swab, show them the soft tip and explain where it needs to be placed and inserted.
For people who do not feel confident to take their own self-collection swab the GP can assist and there’s no need for a speculum, it’s just important that this is still treated as self-collection and needs to be noted as such on the pathology report.
The GP does not need to supervise the collection in itself, but ensure a private place behind a curtain or in the patient toilet for the self-collection to occur, as well as to reassure people that taking their own sample should not hurt.
If the patient drops the swab on a dry surface and/or the end of the swab is touched that’s fine – they can continue to self-collect. But if the swab is dropped on a wet surface, then they’ll need to ask for a new swab and let the GP know.
The GP or practice manager liaises with their local laboratory to find out if they support self-collection or whether they’ll be sending the self-collection on. There are
three large laboratories in Australia that currently support self-collection.
It’s also important that the local laboratory itself provides the general practice with the relevant swabs (validated for the NCSP) – these things need to be in place so that GPs and practices can offer and support self-collection with patients.
Some laboratories also have specifications around the timing for the return of the swab, for example, a GP can determine with the patient the optimum place for self-collection to occur, taking into account the patient’s circumstances.
It may or may not occur in the clinic, it may be appropriate to occur in the patient’s home or at a nursing home or during a home visit. If that’s the case, there needs to be clear instructions to the patient about timely return of the self-collected swab to the lab.
We strongly recommend that these swabs are returned to the practice and then from the practice to the lab. It’s not like patients going to a lab for a blood test and self-collecting there. There needs to be that consultation with their GP so they understand the ramifications of a positive and negative result, and the next steps.
Self-collection is about saving more lives and is a fantastic new change, which will be satisfying for GPs and patients.
The National Cancer Screening Register (NCSR) has a
provider portal, which can support GPs managing patients through the various clinical management pathways in the NCSP. The portal will also contain updated information around self-collection and self-collection pathways.
Cancer Council Australia hosts the NCSR clinical guidelines and has also
published resources supporting the updated guidelines, including a video and FAQs for healthcare providers.
Dr Lara Roeske is a GP with a special interest in women’s health, and member of the National Cervical Screening Program Self-Collection Implementation Committee.
Log in below to join the conversation.
cervical cancer HPV National Cervical Screening Program self-collection
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?