News
Criteria for cervical self-collection tests set to expand
The self-collection pathway will be available to all eligible cervical cancer screening participants from next year, with ongoing GP guidance.
 GPs remain central to guiding patients through self-collection tests for cervical cancer screening.
GPs remain central to guiding patients through self-collection tests for cervical cancer screening.
To improve participation rates and help Australia reach the World Health Organization’s global strategy to eliminate cervical cancer as a public health issue by 2030, the Medical Services Advisory Committee (MSAC) recently called for eligibility criteria to be expanded to all Australian women and people with a cervix.
Coinciding with National Cervical Cancer Awareness Week, Federal Health Minister Greg Hunt recently announced that from 1 July 2022 Australia will be one of the first countries in the world to offer self-collection to all women and people with a cervix through the National Cervical Screening Program (NCSP).
The Cervical Cancer Awareness Week ‘Time to catch up’ campaign aims to remind women aged 25−74 to keep their screening up to date.
It is estimated that Australia will see 913 new diagnoses of cervical cancer in 2021, with close to 237 deaths. Around 80% of cervical cancer cases are detected in women who are overdue for screening, or who have never been screened.
The introduction of GP-guided self-collection for cervical screening has been a ‘game-changer’, helping to address some barriers and under-screening rates.
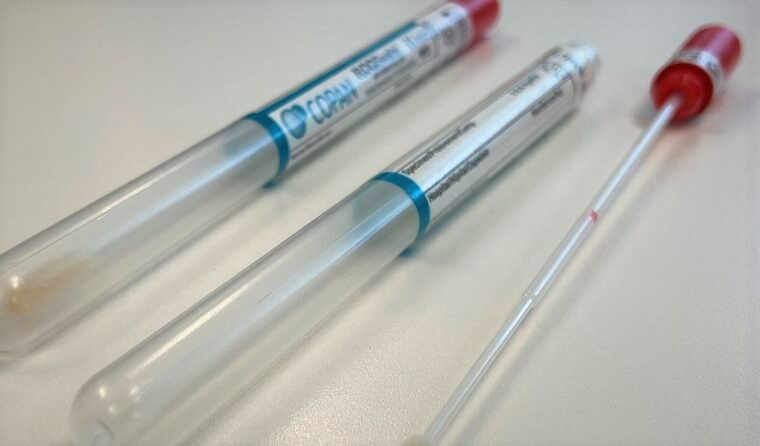
The self-collection pathway is currently only available to women aged 30 years or over, who have never had a human papillomavirus (HPV) test or Pap test, or are two or more years overdue.
Despite the role of screening in early detection and prevention of cervical cancer and the benefits of self-collection, the latest national figures show fewer than 1% of those eligible for self-collection have had such a sample as part of cervical screening.
The time since two-yearly Pap tests were replaced with five-yearly HPV tests at the end of 2017 was anticipated to reduce screening rates, but the impact of COVID-19 also significantly contributed, with lockdowns and a shift away from face-to-face care bringing a significant drop in cervical cancer screening.
Screening rates fell by 67% at the start of the pandemic in April 2020, while rates were still down by 49% in May compared to pre-COVID data.
And more recent data suggests cervical screening rates across some parts of Australia have not returned to pre-COVID levels, with Victoria at 85% of pre-COVID rates and Queensland at 72%.
Self‐collection plays an important role in further reducing the burden of cervical cancer but barriers such as assessing eligibility, inequities in healthcare access, low awareness among eligible participants, and uncertainty about self‐collection among some healthcare providers are keeping rates down.
Dr Lara Roeske, GP, member of the NCSP Self-Collection Expert Advisory Group, and co-author of the National Cervical Screening Guidelines, previously outlined the important role of GPs in supporting patients with cervical screening, including providing access to self-collection kits and guiding patients through the process.
Research indicates that optimum outcomes rely on ensuring GPs are provided with practical advice to support self-collection in their day-to-day practice. This includes being aware of the ‘two different groups’ under the screening pathway changes for women at intermediate risk of significant cervical abnormality, which came into effect on 1 February 2021.
In anticipation of the MSAC recommendations to expand NCSP eligibility criteria for self-collection, now set to take effect from July 2022, consultation has been underway to gain a better understanding of how to best support GPs to comfortably offer self-collection as part of their routine practice.
‘The model of care that Australia has always had for cervical screening places the GP right at the middle of it,’ consultation member and Melbourne University Associate Professor Julia Brotherton recently told newsGP.
‘That connection and trust in the provider is fundamental to engaging women in cervical screening, and the model for self-collect that we have in our program absolutely recognises that.’
VCS Foundation is a key provider of self-collection cervical screening kits. To mark Cervical Cancer Awareness Week, the Australian Centre for the Prevention of Cervical Cancer was launched on 8 November to replace the VCS Foundation.
Professor Marion Saville, Executive Director of the Australian Centre for the Prevention of Cervical Cancer, said the name change reflects the organisation’s primary purpose.
‘Our new name ensures that we are recognised as Australia’s leading organisation in cervical cancer prevention,’ she said. ‘This is an important step to move ahead in the goal to eliminate cervical cancer in our region.
‘We are proud to continue contributing to Australia’s highly successful cervical cancer prevention efforts and to collaborate with partners across the Indo-Pacific region to save thousands more women’s lives.’
Log in below to join the conversation.
Cervical Cancer Awareness Week screening self-collection
newsGP weekly poll
Within general practice, do you think there are barriers to providing flu vaccinations? If so, what are they?