Opinion
How I reduced my opioid prescribing rate
Dr Edwin Kruys decided to scale back prescriptions of opioids two years ago. Here’s how he did it.
 Change is slow – but important, according to Dr Edwin Kruys.
Change is slow – but important, according to Dr Edwin Kruys.
One of my resolutions for 2018 was continuing to reduce my opioid prescription rate for patients with chronic non-cancer pain, in line with RACGP guidelines.
So, two years on, did I put my money where my mouth is?
It isn’t always easy to obtain the required data from our systems, even with the available extraction tools (tips are welcome, of course), but a while back NPS MedicineWise broke the news to me via the mail.
The data suggested that the number of opioids I prescribed per 100 Medicare consultations was seven. The next year it dropped to six, and the following year – last financial year – it was down to five.
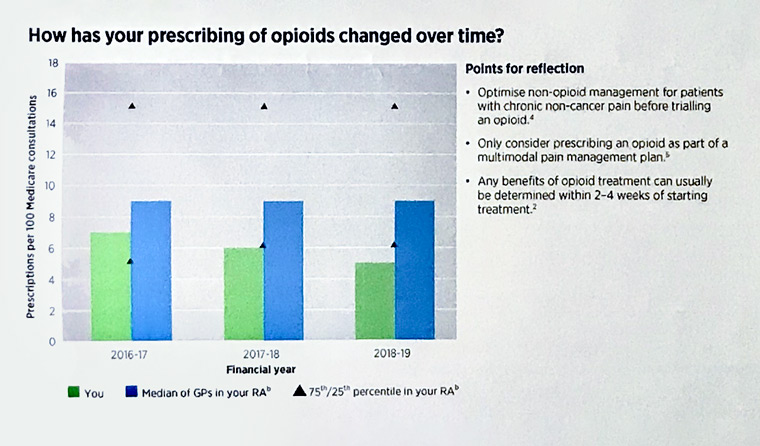
My opioid prescription rate over the past years. (Source: NPS)
How did this happen?
I would like to think that taking the time for conversations about the role of pharmacological and non-pharmacological options has begun to pay off.
Out of the recommended activities to reduce opioid prescribing, I have made a particular effort to apply the following actions:
- Avoid opioids in headache, dysmenorrhoea, dental pains and minor musculoskeletal strains/sprains
- Engage a physiotherapist early for more severe acute musculoskeletal injuries
- If opioids are necessary for severe acute pain, limit prescription to several days’ supply only
- On discharge from hospital, discuss early tapering of opioids as part of the recovery process
- Maximise non-opioid therapies and multidisciplinary care in chronic pain
- Avoid opioids for chronic non-cancer pain in patients with an active or past substance use disorder or unstable psychiatric disorder
- Reassess opioid-responsiveness regularly and often
- Undertake intermittent reductions of opioid dosage
Since making that resolution two years ago, I have spent time practising a
multi-pronged approach to pain management with patients, in which opioids more often play a short-term or last-resort role.
Obviously, there have also been less successful attempts. At times, a patient has not been ready to accept a different approach. Change can be a slow process.
One of the main challenges I have found is the ever-present time constraint in general practice (a reason I am very much in favour of better-remunerated long consultations).
While encouraging, the NPS statistics also raise questions.
For example, have some patients with complex dependency or pain issues been avoiding me? Are they now simply getting their scripts elsewhere?
Overall, though, I can see that data analysis and data-driven quality improvement in general practice is useful.
The NPS opioid prescription information has reinforced my management and approach to pain.
I aim to continue this approach in 2020 – because, as always, there is room for further evaluation and improvement.
Log in below to join the conversation.
opioids pain management prescribing
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?