Column
Australia’s Chief Medical Officer responds to GP questions over opioid warning letter
Professor Brendan Murphy writes for newsGP on last year’s letter warning GPs about high rates of opioid prescribing.
 GPs have previously described the warning letter as ‘intimidating’ and ‘unpleasant’.
GPs have previously described the warning letter as ‘intimidating’ and ‘unpleasant’.
The current trend of opioid use worldwide, including in Australia, poses a significant risk to the health and wellbeing of individuals.
In Australia, approximately twice as many people die from pharmaceutical opioid overdose than from heroin overdose, and opioids are now the most commonly misused pharmaceutical group. The 2016 National Drug Strategy Household Survey found 3.6% of Australians over the age of 14 reported recent misuse of prescription painkillers/analgesics and opioids.
Opioids are, of course, extremely valuable agents in the management of acute pain (including post-operative pain), in palliative care, in chronic cancer pain and in a very limited number of people with persistent non-malignant pain.
However, cumulative evidence has made it clear there is little evidence for the efficacy of long-term opioid use in persistent non-malignant pain, as well as a high incidence of adverse effects from these drugs, including dependency and fatal overdose.
GPs are at the frontline in managing people with chronic non-malignant pain and I fully appreciate the difficulty in managing these patients and meeting their complex needs. It is clear, however, that all doctors must reflect on their prescribing practices if we are to tackle the increasing incidence of harm and death from opioids in Australia.
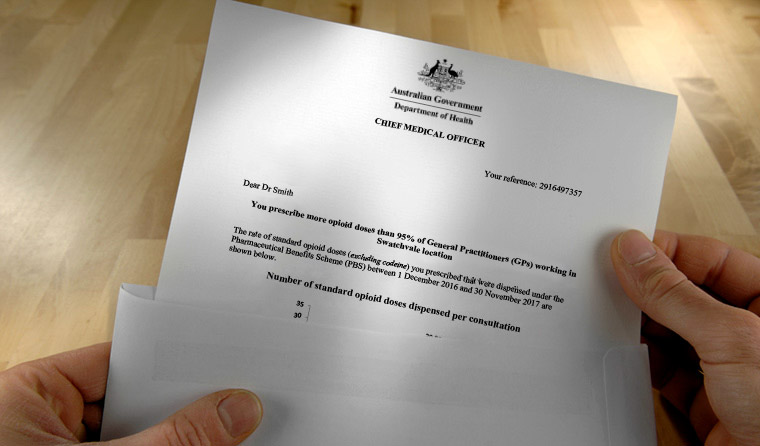
It is for this reason that, in June 2018, I wrote to 4800 GPs who were identified as being in the top 20% of opioid prescribers in Australia – as identified through Pharmaceutical Benefits Scheme (PBS) data.
In this process, it was not possible to identify all GPs working in palliative care or prescribing for palliative care reasons. It was also not possible to identify those GPs who have a specialist pain practice or who have a specific oncology bias to their practice.
Accordingly, these letters were targeted to a broad group of GPs, many of whose opioid prescribing was entirely appropriate for their clinical case mix.
I want to reiterate that we strongly applaud and encourage the work of GPs who are working in palliative care, cancer management and in complex pain clinics. It would be most disappointing and undesirable if any such GPs feel their opioid prescribing practice is anything other than encouraged and supported.
Clearly, in this group of nearly 5000 GPs there are also some who are prescribing, at a higher frequency than their peers, opioid analgesics to patients with chronic non-malignant pain, such as patients with chronic back pain. We know, in the great majority of such patients, these patients’ long-term health is best served if they are weaned off opioids and undertake alternative strategies to manage their pain.
Opioid cessation is complex and needs to be undertaken in a planned way. No one is suggesting that sudden cessation ‘at the direction of government is being required in all cases’. We are simply saying that GPs (and, indeed, all doctors) need to reflect carefully on each and every prescription of opioids for chronic non-malignant pain, other than in a palliative setting.
Some recipients of the letters have raised concerns they may be sanctioned for prescribing opioid medication or that restrictions have been placed on their ability to prescribe opioids. I would like to reassure GPs and patients with these concerns that this is not the case.
There was mention in the letters that, following continued monitoring of prescribing practices, there may be (in rare circumstances) a consideration of some prescribing practices by the Department of Health’s (DoH) Practitioner Review Program (PRP). This would not be done without considering all prescribing and servicing information.
The main purpose of PRP interviews is to understand the reasons for the pattern of prescribing. To date, no practitioners have been referred to the PRP following my letter. Opioid prescribing has come up in only a proportion of cases that have come to the DoH’s attention for other reasons.
The DoH will be evaluating the letters in the coming year. This will help to inform me, and the DoH, on effective strategies to communicate the important role GPs have in tackling this and similar public health issues.
We are certainly aware that these initial letters did cause some anxiety and distress for some GPs, and I apologise for that.
In conclusion, I assure all doctors that appropriate prescription of opioids for acute pain, palliation and cancer pain is supported and encouraged. The huge complexity in management of chronic non-malignant pain is fully acknowledged but, in the light of the compelling evidence of harm, we should all seek to not commence and, where possible, wean and cease the use of opioids in these patients.
For those interested in seeking more information about the letter or resources regarding the use and safety of opioids in clinical practice, further information is available on the DoH website.
chief medical officer opioids prescribing
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?