News
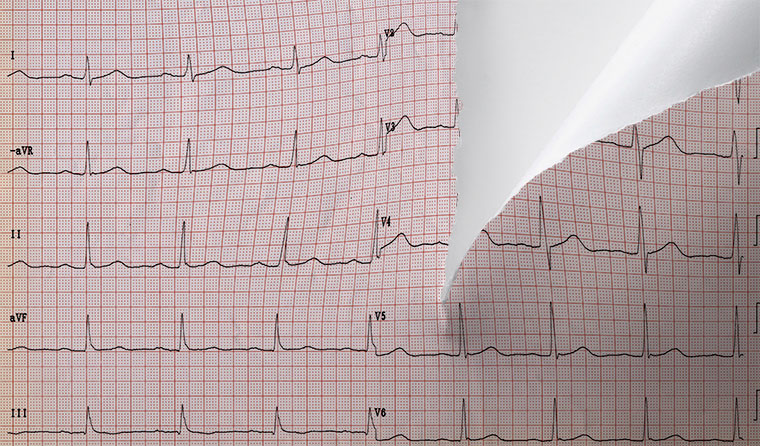
Controversial ECG changes to be reviewed after six months following severe GP backlash
Health authorities have rejected widespread calls to postpone changes to Medicare item numbers for ECGs – but opened the door to a review.
 The move to effectively strip GPs of the ability to bill Medicare for the interpretation of ECGs has been taken as a professional slight.
The move to effectively strip GPs of the ability to bill Medicare for the interpretation of ECGs has been taken as a professional slight.
The changes, which effectively strip GPs of the ability to bill Medicare for the interpretation of electrocardiograms (ECGs), have been slammed by GPs as a threat to the viability of community-based ECG interpretation.
GP-led interpretation of ECGs is seen as a way to relieve pressure on hospital emergency departments and long waiting lists for cardiologists.
The move has been taken as a professional slight and an indirect cut by many GPs.
The changes send a ‘very poor message to general practice’, RACGP Victoria Chair Dr Cameron Loy told newsGP when the changes were introduced.
‘This is an essential part of the curriculum, this is part of our skillset, this is something that we utilise, and it looks like the Government has said that we’re no longer able to do that,’ he said.
The changes come as a GP academic in the field has questioned why an explicit expert recommendation for an ECG interpretation Medicare Benefits Scheme (MBS) item applicable to GPs was seemingly ignored.
Among the 1 August changes are the removal of item number 11700 – which covered 12-lead electrocardiography, tracing and a report – and the introduction of new item numbers such as 11707, which covers GPs but permits tracing only.
The controversy over the changes drew Federal Shadow Health Minister Chris Bowen to make an unusual intervention in the process, joining with the RACGP, the Australian Medical Association (AMA) and the Rural Doctors Association in opposing the changes.
The RACGP also wrote to Department of Health (DoH) Secretary Professor Brendan Murphy to call for an immediate postponement to the changes due to the college’s ‘significant concerns’.
The letter states that the RACGP’s feedback on was disappointingly ‘not considered’. It also points out that reducing support for access to community-based GP-led ECG is unwarranted, as well as poorly timed given the second wave of COVID-19 and concerns over undiagnosed heart disease.
The letter claims the Cardiac Services Clinical Committee (CSCC), which made the recommendations, and the MBS Review Taskforce adopted ‘flawed’ assumptions over geographical variations in use of ECG care, leading to the ‘incorrect assumption’ they represent low value care.
‘There is widespread concern among GPs about the impending changes, with general consensus this is another funding cut for primary healthcare, which may not actually reflect the recommendations of the Committee as recently reported in the medical media,’ the letter states.
‘Reducing the rebate will reduce patient access to this care in the community, unless GPs and practices increase patient out-of-pocket costs.
‘Some practices may no longer offer ECG services, which will require patients to present to other medical specialists and emergency departments.’
Professor Murphy rejected the RACGP’s postponement calls in a letter seen by newsGP, but said he acknowledged the concerns. He also said Federal Health Minister Greg Hunt has ‘agreed to monitor the impact of the ECG changes with a review to be conducted within six months from the date of implementation’.
‘It was the view of the CSCC that some GPs may have inadvertently been claiming referred services for ECG trace and report [item 11700],’ Professor Murphy said in his letter. ‘It was the view of the CSCC it would be preferable to clarify the items and give GPs certainty regarding items they can claim.’
The RACGP consistently defended the right and ability of GPs to interpret ECGs in submissions to the committee investigating the matter in 2017 and 2018.

DoH Secretary Professor Brendan Murphy rejected RACGP call to postpone the changes, but did acknowledge the college’s concerns. (Image: AAP)
Chair of the RACGP Expert Committee – Funding and Health System Reform Dr Michael Wright told newsGP he is ‘very disappointed’ the DoH has pressed ahead with the changes.
‘The department has not taken into account the strong opposition we have provided. But we are pleased to see that Professor Murphy as the new Secretary has agreed to a review of this in six months’ time,’ he said.
‘We will keep resisting changes to the health system that make high-quality general practice less viable.
‘With the MBS review in its final stages, we would urge the DoH to make sure any further changes out of that review are communicated clearly and make sure they don’t further reduce the capacity for practices to provide care at this very difficult time.’
Dr Wright said the timing is particularly disappointing, given the changes have been rolled out in the middle of the coronavirus pandemic.
‘GPs are skilled in performing and interpreting ECGs. It is dangerous if changes to the MBS discourage GPs from performing high-quality care,’ he said. ‘We want to be providing care in the community where patients need it, not sending people unnecessarily to other providers just so they can get a rebate.’
Questions have circled around the decision-making process since the changes were made public, with Minister Hunt defending the move as coming from the MBS Taskforce.
‘It’s the highest clinical advice and it was based on safety,’ Minister Hunt told the ABC (as reported in The Guardian).
A DoH spokeswoman offered a similar explanation, also citing ‘patient safety’ as a rationale to the ABC.
Curiously, the final report of the CSCC clearly recommends the creation of a new MBS item, 11703, which would permit ‘all practitioners’ to claim for the interpretation of ECG results.
This recommendation was not followed, and 11703 was not created.
In an opinion piece in medical media, Professor Richard Harper – who chaired the committee – defended the process and said he had no control over the rebate amount.
‘In developing an item number for GPs, the committee was aware that many GPs had little interest in interpreting ECGs and had not developed the skillset to do so,’ Professor Harper wrote.
In a later article, Professor Harper stated there are ‘no restrictions on GPs performing and interpreting ECGs … the new item [number] 11707 specifically allows this’.
University of Western Australia senior lecturer in general practice Dr Brett Montgomery told newsGP that assertion is only ‘half true’, given the new item number does not cover interpretation.
‘The taskforce report specifically argued for separate item numbers to cover tracing alone … but also an item number to cover tracing plus interpretation,’ he said. ‘This recommendation seems to have been either overlooked or ignored by the department, which is disappointing.
‘I am further disappointed that Professor Harper – the Chair of the committee that authored the report – seems either unaware of this or to be talking around it.’
Dr Montgomery, the author of a recent article in The Conversation on the issue, said many justifications offered by Minister Hunt and the DoH do not seem to be in line with what the report recommended.
‘The Minister and [departmental] spokespeople said they were following the advice of the expert taskforce committee and added it was about safety,’ he wrote. ‘That carries the clear imputation that GP interpretation of ECGs is unsafe.’
Dr Montgomery wrote directly to Minister Hunt on 31 July, asking why he was not following the advice of the MBS Taskforce to introduce the ECG interpretation item relevant to all practitioners.
‘The implicit message here is that GPs aren’t up to this, or that it might be unsafe for GPs to have responsibility for this,’ Dr Montgomery said. ‘That’s what GPs have found insulting and degrading in this whole episode.
‘The question should be, “Why is there no funding for ECG interpretation by GPs?”. Fundamentally, Medicare should be paying for that – and now they’re not doing it.’
The DoH did not respond to questions prior to deadline.
Log in below to join the conversation.
The RACGP is now calling for feedback from members on the impact of the changes for patients requiring ECGs to provide to the DoH for the six-month review. Feedback can be sent to healthreform@racgp.org.au
electrocardiogram item numbers MBS
newsGP weekly poll
How often do patients ask you about weight-loss medications such as semaglutide or tirzepatide?