News
GPs call out ‘ridiculous’ changes to cardiac imaging MBS items
GPs will no longer be able to access item numbers for electrocardiograms that include reporting.
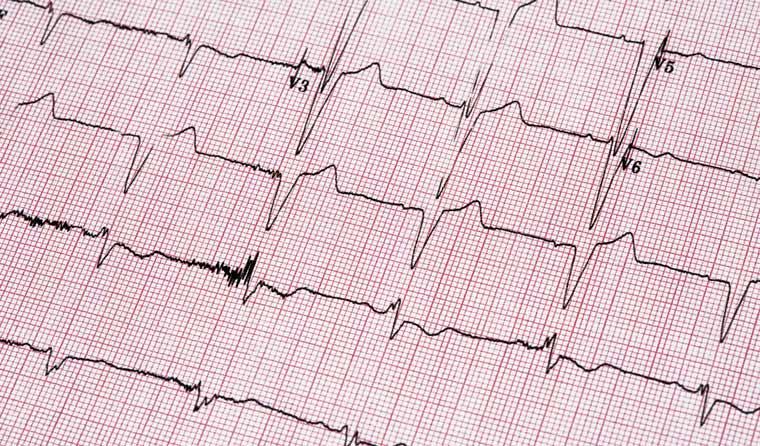 As of 1 August, patient rebates for ECG services provided by GPs will no longer include reporting, with available rebates restricted to item number 11707 (currently 11702) for tracing only.
As of 1 August, patient rebates for ECG services provided by GPs will no longer include reporting, with available rebates restricted to item number 11707 (currently 11702) for tracing only.
‘This is a poor-quality decision, and I think it’s an error.’
That is RACGP Victoria Chair Dr Cameron Loy speaking to newsGP about the new changes to Medicare Benefits Schedule (MBS) item numbers for electrocardiograms (ECGs), which will limit the capacity of GPs.
As of 1 August, patient rebates for ECG services provided by GPs will no longer include reporting, with available rebates restricted to item number 11707 (currently 11702) for tracing only, reimbursed at $19.
GPs will be able to request – but not access – the following items that will need to be accompanied by a referral for a specialist or consultant physician:
- 11704 (currently 11700, 12-lead electrocardiography, tracing and report)
- 11705 (currently 11701, 12-lead electrocardiography, report only where the tracing has been forwarded to a specialist or consultant physician, not in association with a consultation on the same occasion)
- 11714 (12-lead electrocardiography, performing a trace and interpretation)
The changes are based on recommendations made by the 12-Lead Electrocardiogram Working Group of the Cardiac Services Clinical Committee of the MBS Review Taskforce.
The committee did not regard GPs recording of ECG trace results in a patient file as satisfying the report writing element of MBS item 11700, and suggested item 11702 would more clearly reflect GPs’ performance and interpretation of the ECG, as well as ‘ensure appropriate cardiac imaging services are provided to patients’.
The RACGP has strongly opposed the changes since they were first proposed in 2017, holding the position that documenting the ECG outcome in a patient record represented a report, thus satisfying the requirement of item 11700.
In its submission to the MBS review, the college argued that GPs should be allowed to continue to claim item 11700, and that rebates be increased to reflect the true cost of an ECG.
Associate Professor Charlotte Hespe told
newsGP the changes reflect a ‘total lack of understanding’ regarding the role of GPs.
‘We are skilled at both being able to conduct an ECG and interpret an ECG and then act appropriately,’ she said.
‘To say that we just do a trace is basically designating us to a role of technician rather than actually understanding that we have been trained and skilled in this.
‘You do this as a medical student, you do this as a junior doctor, and those are skills that we do every day, and we need to do every day.’
Dr Loy agrees, and says the changes send a ‘very poor message to general practice’.
‘This is an essential part of the curriculum, this is part of our skill set, this is something that we utilise, and it looks like the Government has said that we’re no longer able to do that,’ he said.
‘Or we can do it, we just don’t have an item number that our patients can get a rebate for, which is disappointing.
‘I would have hoped that the knowledge base and skill set of general practice was defined by the medical college in that specialty, and not by some nonsense changed item numbers by the Government.’
While Dr Loy acknowledges the argument that there may have been some over-utilisation of the 11700 item number, he says the approach being taken is not warranted.
‘There have been 2.8 million 11700s activated in the last 11 months, so that’s from July to May. Now that’s not just GPs because that will be cardiologists and geriatricians, all and sundry,’ he said. ‘A lot of ECGs have been done.
‘But the response to that is not to just eliminate the item. There are other ways of doing that, that they could have worked through. This is not the way to manage that problem.’
GPs have raised concerns about the prioritisation of care provided by other specialist medical practitioners, which they believe could lead to delayed diagnoses with significant health and financial consequences for patients, particularly those living in rural and remote areas.
‘They’re saying we have to access a specialised cardiologist to interpret an ECG. That’s ridiculous,’ Associate Professor Hespe said. ‘We all know that the sooner we interpret and act on an AMI [acute myocardial infarction] the better.
‘So if we’re talking about a rural setting, a remote setting, or even an urban setting, quite honestly, where a patient’s presenting in my room, I do an ECG, I can see they’re having an AMI, that’s me interpreting it. So you’re saying that those skills that I have … I shouldn’t be acting on that?
‘I’m sitting here going as a pragmatist, that’s obviously ridiculous.
‘It means it’s going to be increased risk to patients, there’s going to be increased costs to the system, and that’s not okay.’
 Dr Cameron Loy believes the changes send a ‘very poor message to general practice’.
Dr Cameron Loy believes the changes send a ‘very poor message to general practice’.
Dr Loy believes the changes take away a whole raft of opportunities for GPs to help their patients in the ‘cheapest, most efficient part of the healthcare system’.
‘Will GPs just read them anyway and not be able to generate an invoice? I think that’s a shame,’ he said.
‘Are they going to generate a private bill? So increasing out-of-pocket costs on a community that’s already taken an absolute pounding in the last few months with the pandemic?’
‘Or are they just going to say, “Oh well, if the Government says we can’t do it, we’re just going stop doing it?”
‘A whole lot of nonsense is going to occur and a whole lot of people are going to get transferred to emergency departments to read ECGs, which is insanity. So that’s incredibly disappointing, and I think fairly nearsighted and stupid.
‘Once again, there’s been a gouging of money out of primary care, and we already know that some number of billions of dollars has already come out of primary care over recent years. So this is just another one of those.’
Dr Hespe says the decision is bringing Australia one step closer to having an expensive, siloed health care system.
‘It’s really important that GPs know the RACGP never supported this,’ she said.
‘I don’t think that anybody who really knows and understands medical systems and medical care really thinks that it’s just an argument over funding.
‘It’s not okay, because who’s going to suffer? The patients are going to suffer.
‘We need to just really start pulling back and take a vision of what this country actually needs in terms of healthcare systems and the way it’s funded.’
A number of resources outlining the changes are available on the Department of Health website.
Log in below to join the conversation.
cardiac ECG imaging MBS services
newsGP weekly poll
Within general practice, do you think there are barriers to providing flu vaccinations? If so, what are they?