Profile
‘I like to think I’ve made a difference’
For more than two decades, this GP has harnessed a passion for remote health to improve outcomes in disadvantaged communities.
 Dr Lara Wieland with members of some of the remote Aboriginal and Torres Strait Islander communities she feels deeply connected to. (Images: Dr Lara Wieland)
Dr Lara Wieland with members of some of the remote Aboriginal and Torres Strait Islander communities she feels deeply connected to. (Images: Dr Lara Wieland)
Growing up in small towns and spending time outdoors exploring the bush is the childhood imprint that sparked a love of rural life for Dr Lara Wieland.
But while her formative years were split between the Adelaide Hills and idyllic beaches of Cairns, it wasn’t until she first considered working in developing countries that Dr Wieland sparked her interest in remote medicine.
By the time she began studying medicine, that interest had crystalised into a strong determination to provide care in communities where she could help address inequality.
And so, receiving her GP Fellowship in 2001, Dr Wieland started working in Aboriginal and Torres Strait Islander health – a space she has thrived in for most of her career.
‘Working in Indigenous health, I’ve had the privilege of getting to be a part of the lives of my patients living in some very tough situations,’ she told newsGP.
‘I like to think I’ve made a difference for some of them. Earning trust and respect and developing relationships with a community has been very enriching.
‘I really love encouraging and inspiring registrars to work in these areas and I like to think that my experience makes me a good resource and support for them.’
In addition to being an RACGP Fellow, Dr Wieland also has Fellowship with Advanced Rural General Practice and the Australian College of Rural and Remote Medicine, as well as a Graduate Diploma in Rural General Practice (Aboriginal Health).
Meanwhile, living the past 22 years in a farming area in the Atherton Tablelands of Tropical North Queensland, as well as spending time ‘on and off’ in Kowanyama, Cape York, has imparted its own invaluable lessons – especially around solving the ongoing workforce shortages plaguing remote parts of the country.
Ultimately, she believes enhanced public health measures are needed to help reduce the demand on finite services.
‘Workforce has always been a challenge in remote areas but unfortunately it is a challenge everywhere now, which means the politically less influential areas will drop even more to the bottom of the pile,’ she said.
‘We will always be chasing our tails if we don’t see some broader policy based public health initiatives that make a difference to population health.
‘Whilst sugar-laden foods and drinks and fast foods increasingly become the norm and the most easily accessible option for people, and children are being raised on TikTok instead of playing outside, we will only see an increasing tsunami of ill health that we will never keep up with.’
In 2018 Dr Wieland was awarded a Churchill Fellowship to explore retention of doctors in the most remote areas of Canada, where she made ‘striking’ parallels with her own experiences, publishing these findings in the Australian Journal of Rural Health.
‘There are clear similarities in geography, culture, history, etcetera, but also my colleagues and I noted that you can have more in common with a colleague working in remote areas on the other side of the world than with your urban counterparts in your own country,’ she said.
‘I often felt like I was talking to my mirror image when interviewing remote Canadian colleagues. So, I truly believe that the findings from my Churchill report on Canada could very much be applied to Australia.
‘It would also be great to be able to do similar interviews of remote colleagues in Australia, although I suspect the findings would be similar.’
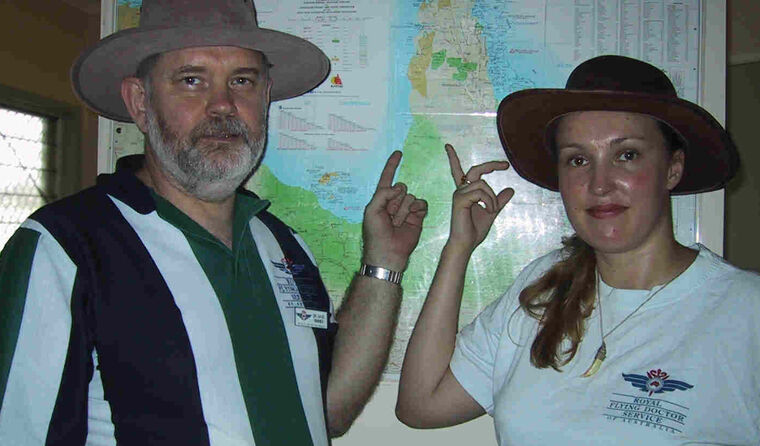 Dr Lara Wieland as a registrar with her supervisor. (Image: Dr Lara Wieland)
Dr Lara Wieland as a registrar with her supervisor. (Image: Dr Lara Wieland)
Alongside her work as a community GP and a stint with the Royal Flying Doctor Service, Dr Wieland has worked as a remote medical educator, senior medical officer at Torres and Cape Health Service and senior lecturer at JCU Medicine and Generalist Medical Training in the Tablelands.
She has also become deeply involved in the Aboriginal and Torres Strait Islander communities she has lived and worked in over the years on many levels, including volunteering with remote youth and as a maternal and child health medical officer at Apunipima Cape York Health Service.
With her wealth of experience and passion embedded in remote general practice and Aboriginal and Torres Strait Islander health, Dr Wieland offers some advice for colleagues considering working in these areas.
‘Don’t get tied down with a big mortgage that ties you in to full-time work for the rest of your life,’ she said.
‘Part time or job share are great options and also give you time to stay connected with friends and family when working remote.
‘Play the long game – if you don’t find balance and pace yourself early you won’t last in the long term. It can be tempting to try and meet all the needs all at once – including trying to keep all your colleagues happy and do all that extra on-call.
‘But better to burn at half-flame for the next 10 years than to go out in a blaze within six months.’
Dr Wieland also encourages people to apply for Rural Generalist training – which is on the way to be formally recognised as a specialist field of medicine – but recommends focusing on the specific skills needed to service the area they want to work in. For example, Advanced Skills Training in Indigenous health or palliative care, rather than the ‘usual’ Rural Generalist Advanced Skills Training.
‘Learn as many skills as you can, be prepared to work in teams and to value all members of your team,’ she said.
‘Have a mentor you can discuss cases or tricky situations with. Never be afraid to ask for advice.’
Having a connection to living in nature since childhood, and now living in the largest wilderness in northern Australia, Dr Wieland says it is ‘incredibly rewarding and exciting’. And while the work can be taxing, having good support and other interests outside of medicine are part of those rewards.
‘Don’t do a job where you sit in a compound after work – get out and get involved in the community and get to know and enjoy the place you work in,’ she said.
‘Have realistic expectations of where you’re going and don’t idealise it. Focus on the positives and the joy that can be found in everyday interactions with patients.’
Log in below to join the conversation.
Aboriginal and Torres Strait Islander health general practice workforce remote GP Rural Generalist
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?