News
‘Nudge’ letters in spotlight amid GP push back on compliance campaign
Concern over the Government approach has seen thousands join the backlash against the latest letter targeting mental and physical health co-claiming.
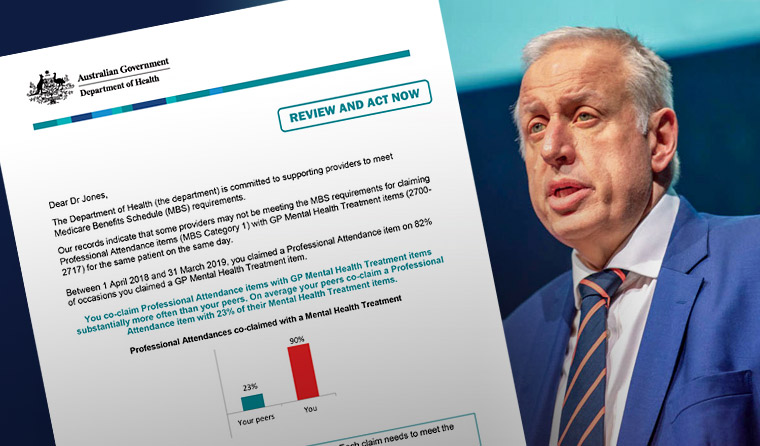 RACGP President Dr Harry Nespolon has described the letter as an ‘intimidating and heavy-handed tactic designed to pick on a small group to affect the whole group’.
RACGP President Dr Harry Nespolon has described the letter as an ‘intimidating and heavy-handed tactic designed to pick on a small group to affect the whole group’.
More than 4000 people have now signed Dr Gillian Riley’s petition, while Melbourne GP Dr Mariam Tokhi has called for an immediate end to the crackdown in The Guardian.
‘While the warnings are ostensibly aimed at GPs “rorting” the system, the effect is to frighten – and punish – family physicians providing whole-person care,’ Dr Tokhi writes.
RACGP President Dr Harry Nespolon has backed critics of the letter, describing it as an ‘intimidating and heavy-handed tactic designed to pick on a small group to affect the whole group’.
The Department of Health (DoH) has moved to address rising concerns, stating that there is ‘absolutely no suggestion that it is not appropriate to treat mental and physical conditions in the same consultation’.
The move is unlikely to mollify angry GPs.
The backlash to last week’s letter comes after the RACGP warned – in a submission to an audit of the DoH’s approach to health provider compliance – of a growing perception among GPs that ‘compliance activities are designed to monitor and target statistical outliers, as opposed to targeting fraudulent activity’.
Dr Michael Wright, Chair of the RACGP Expert Committee – Funding and Health Reform (REC–FHSR), told newsGP the letter has exposed issues regarding the use of algorithms to find outliers within the billing system.
‘Just because you’re a statistical outlier doesn’t mean you’re practising inappropriately,’ he said. ‘We’re trying to make this clear to Medicare.
‘This is the challenge of using algorithms which don’t take into account patient cohorts or practice circumstances.’
In a further sign of the rumbling dissent – made clear on social media and online discussion forums – GP Dr Rebecca Kerr has written an open letter to Federal Health Minister Greg Hunt.
‘I have grave concerns about the very real harm being done to GPs’ mental health and to the general public by the letters being sent to GPs by the government,’ Dr Kerr writes.
‘The level of distress I am seeing amongst GPs in the online community is real, high and appears dangerous. It is interfering with their ability to work and their ability to be with their family.’
Dr Kerr points out that previous DoH compliance letters have failed to take patient cohort and GP-specific circumstances into account.
After receiving a warning letter over her prescribing of the so-called chemical restraint risperidone for a single aged care patient, Dr Kerr decided to simply stop providing services to aged care homes.
‘I was seeing someone with a mental health indication for risperidone ... I got a letter,’ she writes.
‘It was already costing me money being away from the clinic to do this extra service, it was already hard work, with lots of extra phone calls. This letter was the straw that broke the camel’s back. I quit. I don’t provide this service.
‘What does the government see? Success. They ‘“fixed’’ my prescribing. What don’t they see? Reduction in services to the most vulnerable members of the community.’
Dr Kerr argues that the controversial opioid prescribing letter was similarly poorly targeted, and failed to consider GPs with a special interest in palliative care.
Dr Wright said the RACGP is working on the issue.
‘The RACGP is working hard to try and get clarity on these issues and to make sure the different arms of Medicare compliance are providing consistent and clear information for GPs,’ he said.
‘As GPs we treat the whole person. The issue now is that GPs might not deal with a physical problem when someone has a mental health condition, or vice versa, for fear of getting audited by Medicare.’
Dr Wright said the new compliance push will affect how he practices.
‘Frequently, I’ll have a patient for a mental health consultation who also has chronic physical conditions I manage. But I’m now cautious about billing patients for both because I’m concerned I might gain the attention of Medicare compliance.’
To stay safe, Dr Wright recommends ensuring the time and content of all MBS items is met.
‘For most mental health items there is a minimum of 20-minute consultation time. If you only have a 15-minute consultation, you can't be doing a mental health consult, let alone doing both a mental health and physical health item.’
The DoH has told newsGP that targeting holistic care was not the intention of the letter.
‘[The DoH] taken steps to exclude consultations where there was evidence in claiming data that the provider may have been seeing the patient for both mental and physical conditions,’ a spokesperson said.
‘For example, exclusions included where the patient was referred for a pathology or diagnostic imaging service on the same day.
‘This activity is designed to ensure that where this occurs, doctors understand how to appropriately claim Medicare items [and] to provide guidance to GPs to ensure correct claiming of professional attendance items where a mental health treatment item has also been claimed.
‘Recipients have not been requested to provide any evidence to support their claiming; however, they have been advised of the appropriate steps they should take if they do self-identify any incorrect claiming that has occurred.’
Log in below to join the conversation.
compliance Medicare Medicare Benefits Schedule mental health
newsGP weekly poll
As a GP, do you use any resources or visit a healthcare professional to support your own mental health and wellbeing?