News
RACGP President raises concerns after palliative care GP targeted in opioid crackdown
Dr Harry Nespolon has called for a rethink on the DoH’s campaign on opioid prescriptions, warning palliative care patients may be at risk of not getting adequate pain relief.
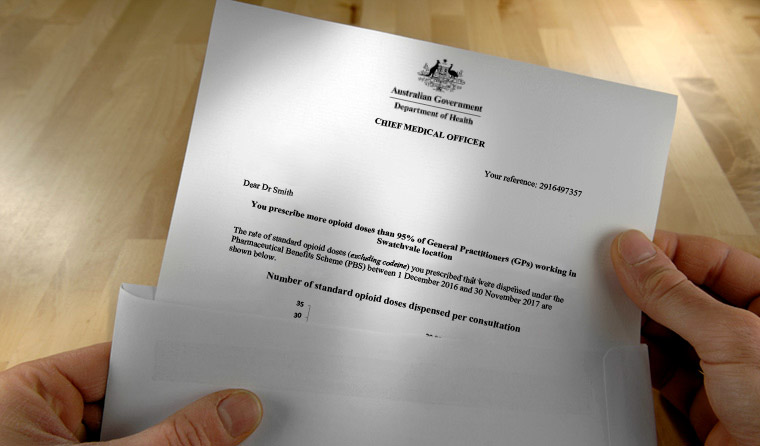 The Department of Health warning letter has previously been described as ‘intimidating’ and ‘unpleasant’.
The Department of Health warning letter has previously been described as ‘intimidating’ and ‘unpleasant’.
The call comes in response to news that a high-profile GP who works in palliative care and aged care facilities has been targeted in the controversial crackdown, in which GPs with high rates of opioid prescriptions are sent a warning letter.
The GP – who does not want to be identified – told newsGP they were surprised at having their prescribing patterns interrogated in a compliance meeting when there were warranted medical indications for prescribing opioids in palliative and aged care.
The GP must now reduce their prescribing within six months or risk potentially career-threatening consequences under a Professional Services Review.
The GP had only recently taken on four new patients whose GPs had also received the letter, and were now refusing to see them.
‘I’m worried that the letter will stop doctors working in the aged care and palliative care space,’ the GP said.
‘GPs are already reluctant to work in that space, and this is yet another reason why GPs may stop or reduce their commitment to this type of work.
‘At the end of the day it is a vulnerable population who will suffer from reduced access to medical care.’
The news led RACGP President Dr Harry Nespolon to call for a rethink on the controversial letter due to the ‘collateral damage’ to patients, and the risk of scaring GPs away from doing much-needed work in palliative care and aged care.
Dr Nespolon warned that the situation could lead to palliative patients not receiving the best possible care.
‘This letter has unfortunately scared a whole lot of doctors who are doing the right thing and giving their patients adequate pain relief,’ he told newsGP.
‘When they ring the Department of Health [DoH], what’s even more concerning is that [the department] has not been reassuring about what the next steps are going to be. It’s caused significant collateral damage.’
Dr Nespolon said the DoH needs to either become more sophisticated in how it sends out the letters, or introduce a separate Medicare line item for patients receiving palliative care to improve the quality of data.
‘There’s evidence that patients with non-cancer pain don’t benefit from high doses of opioids, so we should all be reviewing our practice in that area. But those who are in the palliation stage should be getting more,’ he said.
The RACGP last year warned the DoH that GPs working in palliative care and aged care could be wrongly targeted due to their need to prescribe opioids for these patient cohorts.
Following this, newsGP reported that several GPs had – or were considering – pulling back from palliative care out of fear for their livelihoods after receiving the letter.

RACGP President Dr Harry Nespolon has called for a rethink of a controversial DoH letter warning GPs about high rates of opioid prescription.
After the letter campaign rolled out last year, the DoH moved to reassure GPs that areas in which higher rates of opioid prescription are common – including palliative care and aged care – would be taken into account.
The high-profile GP presented the DoH with evidence of their case mix, as well as detailed evidence from a clinical audit showing quality process for prescribing.
‘Patients with complex and chronic conditions, people who are housebound because of physical issues, palliative care and end of life, and aged care – these are the only patients I see,’ the GP said.
‘I outlined my approach, my practice, and the reasons for prescribing opioids and that almost all of the patients had input from other appropriate clinicians such as a geriatrician, or from an RMMR [Residential Medication Management Review] and pain assessments.
‘I got a letter back saying they still had concerns around my opioid prescribing based on the fact that my peers may consider my prescribing to be inappropriate. Ironically, many patients are increasingly referred to me by my peers to take over their care.
‘The comparison was with all active GPs, not those with a specialised practice such as mine.’
The GP was told that comparison data for GPs with a similar practice was not available.
‘The context around palliative care needs of this cohort of patients appears not to be appreciated. My prescribing for the majority of my patients on opioids is very low dose and all in residential aged care settings,’ the GP said.
‘Of course we need to address the opioid problem and ensure quality of our prescribing – but in a formative way, not a heavy-handed policing that risks potential unintended consequences.
‘The issue we want to be addressing is unwarranted variation, not warranted variation. It’s an important distinction that seems to be completely overlooked.’
If the GP’s prescribing does not change after the monitoring period, a referral to Professional Services Review may occur.
‘The potential consequences are pretty significant,’ the GP said.
The news comes after a survey last year found more than a third of doctors planned to cut back or stop aged care facility visits due to concerns about poor staffing ratios and low remuneration.
A DoH spokesperson told newsGP the warning letters were a one-off, and that the RACGP and Australian Medical Association (AMA) and other professional bodies were consulted on the design of the letters.
‘The letters were intended to promote reflection on each GP’s prescribing, with the clear message that in many cases prescribing was appropriate. It is unfortunate that some GPs may have misinterpreted the letter as a definitive criticism of their prescribing practice,’ the spokesperson said.
‘Though palliative care-specific items were excluded from the exercise, the [DoH] noted at the time that it was not possible to identify all GPs working in palliative care from the available data.
‘The letters therefore specifically acknowledged that practitioners working in this area who received the letters may decide that their prescribing was appropriate and need take no further action. The letters were intended simply to promote reflection on each GP’s prescribing.
‘The [DoH] always welcomes input from the RACGP and other stakeholders, and would welcome the opportunity to discuss ways to support appropriate GP care in aged care and palliative care settings.’
The DoH does not yet have data on whether the letters have led to a reduction in opioid prescriptions.
Palliative Care Australia (PCA) nurse practitioner clinical adviser Kate Reed told newsGP her organisation is becoming increasingly concerned that palliative patients are getting caught up in the crackdown.
‘GPs will pull out, and there are just not enough specialist palliative care practitioners to pick it all up. It makes an under-served population more vulnerable,’ she said.
‘Palliative care is a human right, according to the World Health Organization.’
aged care department of health opioids palliative care
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?