News
What does the Medicare integrity report mean for GPs?
The 77-page independent review has been published. Here, newsGP sums up some of the key implications for general practice.
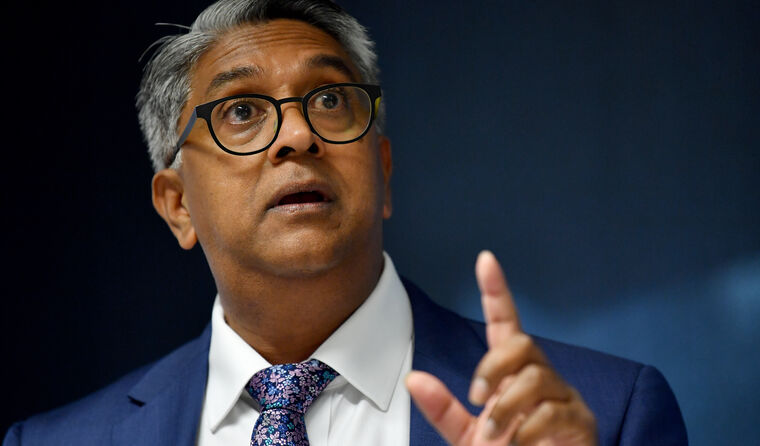 The author of the report, health economist Dr Pradeep Philip, has said Medicare needs significant change. (Image: AAP Photos/Bianca De Marchi)
The author of the report, health economist Dr Pradeep Philip, has said Medicare needs significant change. (Image: AAP Photos/Bianca De Marchi)
‘Not currently fit for purpose’: those are the words in a newly-released independent review into Medicare that could be the precursor to major change for the system used by GPs around the country.
The Independent Review of Medicare Integrity and Compliance report was published on Tuesday after being commissioned in November by Federal Health and Aged Care Minister Mark Butler following extended and often heatedly contested media coverage on Medicare.
Addressing the widespread rort and non-compliance claims that prompted the review, its author – health economist Dr Pradeep Philip – noted that ‘the overwhelming majority of practitioners’ are ‘well-meaning and protective’ of the care they provide to patients.
He also attributed ‘a large part of the success and efficacy of Australia’s health system’ to that type of altruistic behaviour’, while simultaneously describing a ‘disproportionate’ fear of the Professional Services Review.
There is no conclusion in the report about the exact level of current non-compliance, but Dr Philip states that $1.5–3 billion is ‘entirely feasible’ using a conservative definition of non-compliance and fraud.
The report calls for a significant overhaul of a system he says has not evolved sufficiently to cater for different technologies and business models, nor the changing way of delivering increasingly complex healthcare.
‘At the core of all this … lies the complexity of the system, the lack of clarity of many aspects of the compliance system, the lack of emphasis in decision support pre-claims and pre-payment, and the lack of continuous monitoring,’ he wrote.
In his report, Dr Philip warned of growing systemic vulnerabilities that will require ‘significant attention’ if the risk of rising fraud levels is to be avoided.
The review includes 23 recommendations, grouped into four broad categories: governance and structure, operational processes, modernising technology and strengthening legislation.
What are the key points for GPs?
Dr Philip identifies deep flaws with the existing system, and in a recommendation that is particularly pertinent to general practice, he says improvements in education need to happen.
This is a position long held by the college, which
in its submission to Dr Philip advocated for ‘educative processes focusing on prevention of incorrect claiming, rather than punitive measures and blunt instruments’.
In recognising an ‘overly fragmented, disjointed’ system, Dr Philip states that clear rules and a greater focus on pre-claim and pre-payments are needed to address non-compliance and fraud.
‘Changes occur to these items at a frequency which is difficult for individual practitioners to keep up with,’ he wrote, noting that around 3000 Medicare items have changed in the past 2–3 years.
‘In this environment, communication of changes to health professionals themselves needs to improve.’
The report recommends that a ‘comprehensive system for continuously improving and updating education and awareness for providers regarding the application and use of the MBS must be introduced, including the involvement of key stakeholders’.
Specifically, Dr Philip recommends expanding the use of practical case studies, as well as closer collaboration between government agencies and peak bodies in the preparation of education materials.
He also advocates expanding education to include corporate entities and administrative staff involved in preparing MBS claims.
A further recommendation suggests the ‘ongoing tailoring of the education and reference materials available to providers and patients to support compliant MBS claiming’, as well as ‘participation in face-to-face seminars and education events for target groups’.
In another recommendation that may be welcomed by GPs frustrated with the complexity of the system – subject to more detail being put together – Dr Philip says restructuring the design and composition of MBS numbers should be considered.
This could occur by using ‘a time-based backbone together with additional specific intervention and procedure codes, bundling of co-claimed surgical items to create single procedure codes, and integration of pre-claim decision support into practice management software’.
He also notes ‘questions of process and fairness’ in the current compliance system, including the lack of timeliness and the administrative burden, which he said causes unnecessary ‘fear’ among health practitioners.
What about the $8 billion fraud and non-compliance claim?
As noted above, Dr Philip did not land on a specific figure beyond stating that a figure from $1.5–3 billion is ‘entirely feasible’.
He states that calculating the true scale of non-compliance ‘is limited by data availability’ and linkage ‘challenges then muddied by differences in definitions’, and urges policy makers to look beyond the contested figure.
‘To reiterate, there is greater value to be gained from a focus on the structural recommendations in this review than on the numeric value debate that has been a focus of public discourse to date,’ he wrote.
‘Stamping out fraud and reducing non-compliance must be the focus of system reform.’
However, he notes that Dr Margaret Faux, who was consulted for the review, has since adjusted her estimate of $8 billion non-compliance – which was widely reported last year – to $10 billion.
Dr Philip said there are ‘methodological issues and definitional challenges’ with her estimate, but warns that fraud could reach the levels described by Dr Faux if action is not taken.
The report only obliquely references
the considerable distress caused to many GPs by the coverage.
‘I am also conscious that there are wider impacts of these sorts of discussions and debates and that a number of key participants in the health system have taken offence to the claims of entrenched, intentioned, and significant fraud in the system,’ Dr Philip wrote.
‘The semantics and specifics of language, how we talk about these issues, and how we debate and draw on evidence, should focus on the arguments not the person and be constructive.’
What next?
Upon releasing the report on Tuesday, the Department of Health and Aged Care said the Government will work with health professionals, patients and peak bodies in considering a comprehensive response.
However, the broad range of the recommendations involved and their likely associated costs are a potential stumbling block, with Dr Philip describing the need for ‘major investment in modernising the platform and compliance tools and techniques’.
He also suggests that reforms should be worked in to fit in with the development of
the Strengthening Medicare Taskforce report, which was carried out separately.
‘Moving the culture of Medicare integrity towards a better balance between continuous quality and safety improvement and the detection of non-compliance and fraud, will promote more buy in to reform,’ he wrote.
‘[It will also] support retention of those parts of the experienced clinical workforce necessary to support a safety culture at a time when many are considering earlier retirement or have retired.’
The full Independent Review of Medicare Integrity and Compliance on the Department of Health and Aged Care website.
Log in below to join the conversation.
MBS Medicare Medicare Compliance RACGP Strengthening Medicare Taskforce
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?