News
Corticosteroid recommended for COVID-19 patients
newsGP speaks with the Executive Director of Australia’s National COVID-19 Clinical Evidence Taskforce about its latest recommendation.
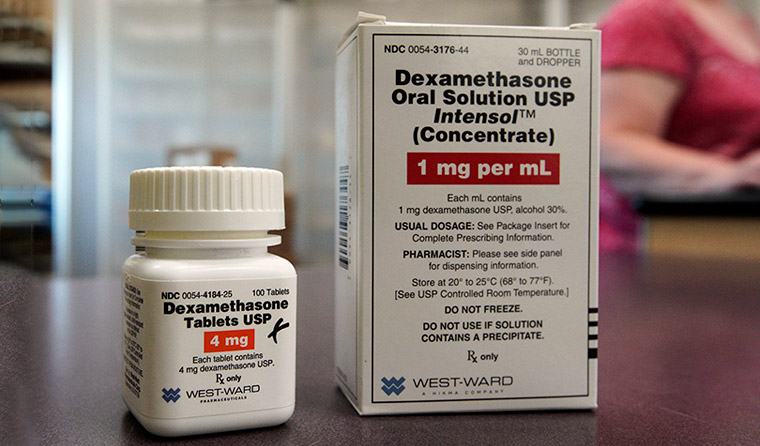 Corticosteroid dexamethasone has a well-established pharmacological profile that is already used to treat a range of conditions. (Image: AAP)
Corticosteroid dexamethasone has a well-established pharmacological profile that is already used to treat a range of conditions. (Image: AAP)
‘This is the first time we have a treatment that has been shown to reduce mortality in people with COVID-19.’
That is Associate Professor Julian Elliott, an infectious diseases expert and Executive Director of Australia’s National COVID-19 Clinical Evidence Taskforce (the taskforce), referring to the latest recommendation for the use of dexamethasone.
The corticosteroid is specifically recommended for patients in Australia the coronavirus who are receiving oxygen or mechanical ventilation.
It is recommended that practitioners consider using 6 mg of dexamethasone daily, either intravenously or orally, for up to 10 days in adults with COVID-19.
‘It’s noteworthy that this drug is very widely available, affordable, [and] its safety profile is very well-known. So the implementation of this recommendation is not as difficult as with remdesivir,’ Associate Professor Elliott told newsGP.
‘This treatment could save the lives of patients in Australia who are seriously unwell with COVID-19.’
The taskforce’s recommendation is based on data released on 16 June from the RECOVERY (Randomised Evaluation of COVid-19 thERapY) trial led by researchers at the University of Oxford in collaboration with multiple hospitals around the UK.
In the dexamethasone arm of the trial, 2104 patients were randomised to receive a low-dose of the corticosteroid. They were then compared to 4321 patients who did not receive it.
Among those who received the drug, patients requiring oxygen had a 14% reduced risk of death, and ventilated patients a 29% reduction.
There is no evidence to suggest dexamethasone prevents people from contracting the virus. It is understood the drug is effective against the virus due to its anti-inflammatory effects.
‘The hypothesis is that by reducing inflammation, that reduces the secondary harmful effects of inflammation in the patients with more severe COVID-19,’ Associate Professor Elliott said.
‘So the fact that the greatest mortality benefits accrue to those who are sickest tends to support that.
‘There was also no benefits seen in those who did not require oxygen, and that would also support that hypothesis.’
But the infectious diseases expert is keen to point out that the recommendation is conditional, as it is currently based on preprint data that has yet to be peer-reviewed.
Given the drug’s well-established pharmacological profile, however, as well as the fact it is already in use to treat a range of other conditions, the taskforce sees the recommendation as a significant step forward.
In the three weeks since the preliminary data was released, a surge in demand has already been noted.
World Health Organization (WHO) Director-General Tedros Adhanom Ghebreyesus agrees the findings offer a ‘much-needed reason to celebrate’, but urged people to be ‘guided by solidarity’ to ensure countries with high numbers of critically ill patients could be prioritised, as well as allowing for enough supply to treat other diseases.
‘The next challenge is to increase production and rapidly and equitably distribute dexamethasone worldwide, focusing on where it is needed most,’ Mr Tedros said during a media briefing in Geneva.
‘Fortunately, this is an inexpensive medicine and there are many dexamethasone manufacturers worldwide, who we are confident can accelerate production.’
Meanwhile, the taskforce has reassured expectant mothers with COVID-19 on the risk of exposure to their newborn baby via vertical transmission. Based on available data, a conditional recommendation has been made for the mode of birth to ‘continue as per usual’.
‘There has been discussion and controversy over the last few months about risk of vertical transmission, and I’m sure we’ll be learning more in the coming months,’ Associate Professor Elliott said.
‘But there’s no evidence to indicate that caesarian section for women with COVID-19 reduces the risk of vertical transmission to the newborn.’
Given the respiratory deterioration that can occur as a result of virus, the taskforce does note that it may prompt urgent delivery on an individual basis.
Established in April, the taskforce has grown to have almost 200 clinicians involved on its panels and, much like Australia’s health system, is now much better prepared for the pandemic than it was a few months ago.
‘The last, say, couple of months, when people have felt like the urgency in Australia was perhaps waning, we did not stop,’ Associate Professor Elliott said.
‘Our panels have continued to work very hard because so much of this is our preparedness and we are of course aware that there could be a further increase in cases.’
Victoria recorded 127 new cases on Monday 6 July – its highest daily increase since the pandemic started. A man aged in his 90s died of the virus in hospital overnight, with another man in his 60s dying on Monday morning.
The country’s death toll now stands at 106.
With 645 active cases in the state, the NSW–Victoria border will close at midnight on Tuesday 7 July for the first time in 100 years.
Twelve postcodes have returned to stage-three restrictions, while nine public housing towers have been put into
complete lockdown for at least five days, with residents restricted from leaving the premises.
Despite the rising numbers, Associate Professor Elliott believes Australia’s response to the global health crisis has been ‘very strong’.
‘Government and community take it very seriously and continue to respond appropriately … we’re just dealing with a virus that is quite infectious,’ he said.
‘[But] Australia has demonstrated that we can dramatically reduce transmission with full lockdown, and we’re now in a phase in Victoria where we will see whether more targeted approaches can also reduce transmission.’
Associate Professor Elliott is
among the experts calling for the establishment of an international coalition for behaviour and social preparedness with a focus on non-medical methods of cutting viral transmission rates.
‘The way our research systems work, there tends to be quite a lot of focus on drug treatments and, as we’ve seen to date, a lot of the most important responses to the pandemic have been behavioral,’ he said.
‘Yet we have relatively little research funded or conducted around the behavior change that is a foundation for the response to the pandemic.’
The taskforce will continue to update its
clinical guidelines for COVID-19 weekly.
Log in below to join the conversation.
clinical recommendations coronavirus dexamethasone
newsGP weekly poll
Which of the following areas are you more likely to discuss during a routine consultation?