News
Evidence suggests AstraZeneca and Pfizer are equally effective
Experts say the research is reassuring, and indicates that both COVID vaccines offer a pathway to Australia reaching a high level of immunity.
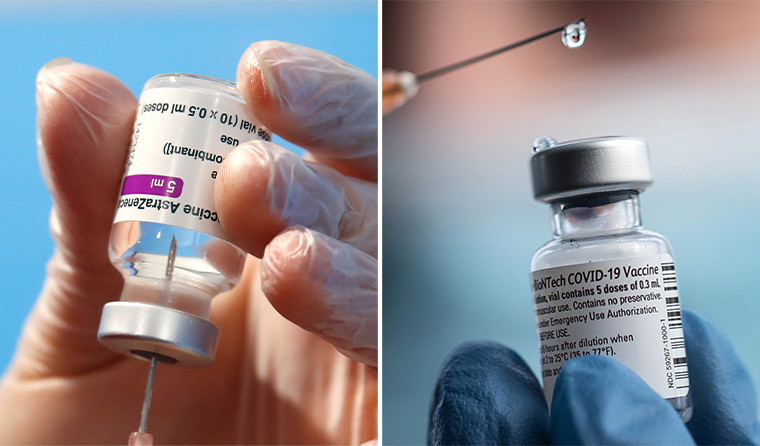 Contrary to clinical trial data, the real-world experience in the UK shows no difference in the level of protection offered by the AstraZeneca and Pfizer vaccines against COVID.
Contrary to clinical trial data, the real-world experience in the UK shows no difference in the level of protection offered by the AstraZeneca and Pfizer vaccines against COVID.
A surprising development of Australia’s efforts to combat the coronavirus pandemic has been a vaccine brand battle of sorts – AstraZeneca versus Pfizer.
It started with reports of efficacy rates from phase 3 clinical trials and came into full force as reports emerged over blood clot concerns.
But a pre-print study from the UK, recently uploaded to medRxiv, has found that real-world data suggest both Pfizer and AstraZeneca vaccines are equally effective, with no real difference in the level of protection offered.
The research involved 373,402 participants, and saw 1,610,562 polymerase chain reaction (PCR) tests conducted between 1 December and 3 April.
The results revealed the odds of being infected after two doses of either vaccine were reduced by 70% compared to unvaccinated individuals without evidence of prior infection, with no evidence that the benefits varied between the AstraZeneca and Pfizer vaccines.
With the two vaccines currently in circulation in Australia, Dr Kylie Quinn, Group Head and Research Fellow at RMIT’s School of Health and Biomedical Science, told newsGP the results are good news.
‘This is the kind of real-world data that we need to really understand how these vaccines perform,’ she said.
‘How things perform in a clinical trial don’t always equate to how they perform in the world, so it gives us confidence that these vaccines, in this study, performed equally as well in terms of preventing disease and they’re hitting the mark in a number of ways.’
Associate Professor James Wood, a leading vaccine expert at the University of New South Wales, agrees, and says the findings provide reassurance Australia is on the right path.
‘It does present herd immunity as a much more achievable proposition in Australia with our vaccine mix,’ he told Nine Newspapers.
‘With the caveat we don’t know what we’ll be seeing in six months’ time.’
The study also demonstrated that the vaccines are around 65% effective more than 21 days after just one dose of either vaccine, and that those who do get infected have milder symptoms.
‘So that means that, potentially, they’re less likely to pass that virus on to people around them,’ Dr Quinn said.
‘So it’s a way of protecting not only yourself, but also people around you, which is super important.
‘[However], protection does trend slightly lower for older people [aged 75 and over] if they’ve just had one dose of the vaccine. So that’s a really important part … that GPs can be communicating to their older patients, that that second dose is really important for them to get up to the same level of immunity that we would see in younger individuals.’
While positive news, it does raise questions over the disparity in efficacy rates reported from phase 3 clinical trials, at least for Pfizer, which came in at 95%, along with other recent real-world data out of Israel.
Dr Quinn says while it is interesting that it isn’t entirely surprising.
‘We do expect some adjustment of those numbers, as efficacy doesn’t always equate to effectiveness,’ she said.
‘So that’s always something that you keep in mind and you want to monitor as you roll a vaccine out.
‘A lot of those really early clinical trials were coming out when we didn’t have a lot of these variants of concern circulating … so part of it could be the variants.’
As well as accounting for emerging variants, Dr Quinn says different characteristics in population groups being studied, such as age, can also play a role, as can the criteria being used to define whether someone is sick or not.
‘So you’re not comparing apples to apples – you’re comparing different trials,’ she said.
‘There’s lots of different factors that can impact those numbers and it’s really hard to pin it down to one.’
Meanwhile, a separate Israeli study, published in JAMA, estimated that the Pfizer vaccine is 97% effective against symptomatic infection and 86% against asymptomatic infection among healthcare workers.
More than seven days after receiving the second dose of the vaccine, eight symptomatic and 19 asymptomatic infections were recorded among 5517 fully vaccinated workers compared to 38 symptomatic and 17 asymptomatic cases in 757 unvaccinated workers.
Yet another recent study published in JAMA, this time out of the US, showed vaccination with Pfizer reduced the risk of both asymptomatic and symptomatic infection by 96% in fully vaccinated healthcare workers at a hospital in Memphis, compared with unvaccinated workers.
That number reduced to 90% for asymptomatic infections alone.
While all Australians over the age of 50 are now eligible to be vaccinated, a poll from April shows that less than 50% are willing to get the AstraZeneca vaccine.
But Dr Quinn says she hopes the UK research will assist GPs in addressing any hesitancy among their patients.
‘It gives them some real-world information from people who have rolled this vaccine out,’ she said.
‘These were the experiences of more than 300,000 people in the UK, and so it really does illustrate that these vaccines are highly protective – both of them – and either of them are really good options.
‘We have this transition ahead of us, integrating back into the international environment, and it’s really important to protect ourselves as individuals, and to also protect folks around us, [that] we have a high level of immunity within our community, and both of those vaccines are a pathway to that.’
Log in below to join the conversation.
AstraZeneca coronavirus COVID-19 Pfizer vaccination vaccine rollout variants
newsGP weekly poll
As a GP, do you use any resources or visit a healthcare professional to support your own mental health and wellbeing?