News
Vaccination gap: Vulnerable communities left exposed as Omicron threatens
Aboriginal and Torres Strait Islander COVID vaccination rates continue to lag the general population, with some areas still less than 50% fully vaccinated.
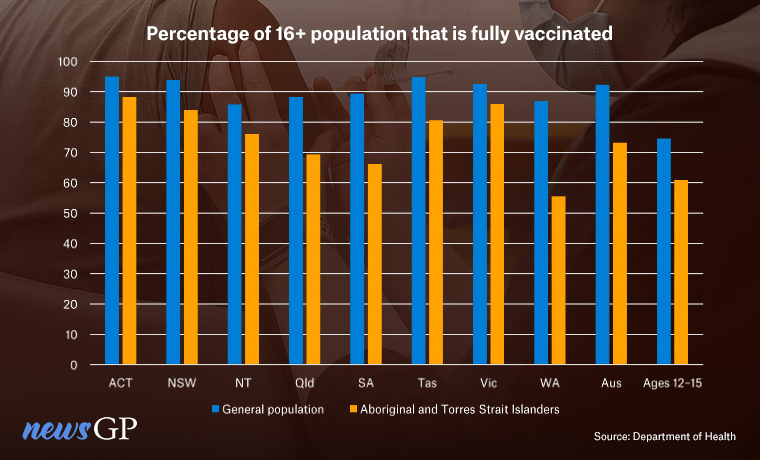 Aboriginal and Torres Strait Islander vaccination rates are behind the general population in every state and territory.
Aboriginal and Torres Strait Islander vaccination rates are behind the general population in every state and territory.
With 92.3% of people over 16 having received at least two doses of a COVID vaccine, Australia has one of the highest vaccination rates in the world.
But once again, its Indigenous people are being left behind.
Despite numerous warnings and requests for help, the vaccination gap between the general population and Aboriginal and Torres Strait Islanders remains, with only 73.2% of over-16s fully vaccinated as of 12 January.
The difference is most pronounced in Western Australia, which has so far been relatively untouched by COVID but has a vaccination gap of more than 30%.
All of the local government areas (LGAs) in which less than half of the Indigenous population is fully vaccinated – including the Shire of Derby-West Kimberley (41.4%) – are also in WA, despite the general population in many of those areas posting rates above 85%.
Dr Nalini Rao runs the only general practice and pharmacy in Mullewa, a small town 450 km north of Perth of around 700 people, 47% of which are Aboriginal.
She told newsGP that hesitancy, complacency and a lack of tailored public health messaging have hampered local vaccination efforts, as have issues with securing sufficient mRNA vaccines.
‘There was a lot of anxiety at the start, especially regarding AstraZeneca,’ she said.
‘For some unknown reason, I was not approved for Pfizer until several months after [nearby town] Morawa, which has only a 10% Aboriginal population. Same for Moderna.
‘Most came in for Pfizer once it was approved … [but] the supply issue is still concerning.’
Via a series out outreach clinics and local vaccination events Dr Nalini says her clinic has managed to vaccinate roughly half of the town’s Aboriginal population, but she fears what will happen once Omicron inevitably arrives.
‘I’ve been on a small holiday but go back on the 17th and expect to be bombarded. With the imminent [border] opening on 5 February, the urgency is increasing,’ she said.
‘I don’t have a practice nurse and also run the pharmacy out of my practice. The practice assistant, the pharmacy assistant and I work through lunch most days to accommodate walk-ins for COVID jabs.
‘We have managed to keep up with demand by all means possible, but the rest of my holidays will be spent studying RACGP guidelines on managing COVID patients in the community … I am dreading 5 February.’
But while supply may partly explain the issues Dr Rao has faced, statistics from other parts of the country suggest there is more than geography and remoteness at play.
Greater Geraldton, a town of more than 30,000 people 45 minutes west of Mullewa has fully vaccinated 91.1% of its population over 16, but only 49.5% of its Aboriginal and Torres Strait Islanders.
There are also examples within Perth itself. The City of Swan has an overall vaccination rate of 88.2%, whereas only 56.5% of the more than 3500 Indigenous people living there are fully vaccinated. Meanwhile, Gosnells is 86.9% fully vaccinated but just 55.2% of its Aboriginal population have received two doses.
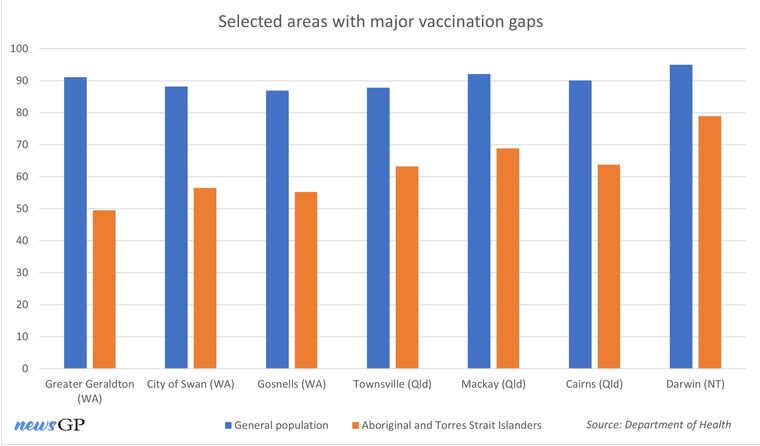
Numerous local government areas in Australia have substantial differences in the vaccination rates between the general population and Aboriginal and Torres Strait Islanders.
Wiradjuri man and RACGP Aboriginal and Torres Strait Islander Faculty Chair Professor Peter O’Mara told newsGP many of the problems stem from government not prioritising Indigenous Australians enough throughout the rollout.
‘They acknowledged that we were high risk but didn’t really take action and I think that’s really disappointing,’ he said.
‘They did around some of the other populations – like elderly people and people in residential aged care facilities, and of course they should have done that as well – but part of my concern from the beginning was that we needed to change the narrative, because Indigenous people were just tacked on to the end of conversations.
‘I never really heard anything significant about “this is what we need to do” from the government in terms of working with our communities.’
Professor O’Mara says tailored messaging and outreach programs, like those conducted in Mullewa by Dr Rao’s practice, are vital for closing the gap.
‘One of the things that we’ve seen in central Australia is that when we get community elders to have a good understanding of the importance of the vaccination, then the vaccination rates in those communities go up significantly,’ he said.
‘Where I work at Tobwabba Aboriginal Corporation Medical Service, our rates are really high … it’s about connection to the community and spreading that message.
‘Once we got the vaccines in, it was just about going and having a one-on-one with community members about how important it is, and then they would then share that message with other community members to get the rates right up.’
Such an approach can be just as effective in metropolitan settings, Professor O’Mara says, provided the programs and the messaging are tailored to the leaders and people who live there.
‘I think the networks are thicker in those communities,’ he said. ‘The information flows and we talk about the “Koori Grapevine” as a way of getting messages around.
‘In those cities it’s probably every bit as easy as it is in rural places, because even though the numbers are higher, the message spreads wider.’
A WA Health Department spokesperson told newsGP increasing vaccination rates among Aboriginal communities is of ‘the utmost importance’ and a key area of focus for the state’s vaccine program.
‘As a society, we have a responsibility to protect and safeguard our Aboriginal people and communities, so they can remain safe and strong,’ the spokesperson said.
‘While there are many reasons as to why certain groups or individuals may be hesitant to be vaccinated, all efforts are made to engage with stakeholders and communities across the state, and continue to bring more opportunities for COVID-19 vaccinations.’
The spokesperson also referenced the Keeping Culture Safe and Strong: Vaccination Focus program – launched in late November 2021 – as part of government efforts to increase Aboriginal vaccination rates.
While COVID is yet to take hold in Western Australia to the same extent as it has in other parts of the country, Far North Queensland could offer a clue as to what Aboriginal people can expect once the border opens should the vaccination rates remain low.
Townsville-based RACGP Rural Chair Dr Michael Clements told newsGP the Omicron wave has quickly taken over the city of nearly 180,000 residents, to the point where he says it is ‘everywhere, just everywhere’.
‘We are seeing sick kids … there are long wait times at the emergency department, and the fact that they’ve cancelled outpatient appointments and things like that is alarming – that is a disaster,’ he said.
‘If they’re not doing the usual work, then that actually means that they’re not coping and they’re doing very poorly.
‘We always thought that having cases in your community and seeing your own loved ones get infected would be a final push. And it has to a certain extent, but sadly, it hasn’t really converted as many into getting vaccinated as we’d hoped.’
Townsville itself is 87.8% fully vaccinated, but the Aboriginal and Torres Strait Islander population again trails at just 63.2%. Like Professor O’Mara, Dr Clements believes the shortfall is due in-part to a lack of tailored messaging on behalf of health authorities, but he also says this oversight is a symptom of long-term systemic issues.
‘It’s not a gap because of lack of access, because the vaccines have certainly been available to the whole community,’ he said.
‘What these pandemics do is show weaknesses in our overall system and our overall health system has been failing our First Nations people … we’ve been talking about closing the gap for years, but we haven’t.
‘I personally see the low vaccination rates as a side effect of the failure of the [Federal Department of Health] to deliver culturally appropriate, effective and efficient care over the past 10 years.’
In order to solve the issue, Dr Clements says more funding is required.
‘The way that the Federal Government has structured and funded the rollout … means that practices will focus on high volume clinics, which is not culturally appropriate care,’ he said.
‘The lack of funding means there’s a reduced incentive to actually seek out [hard-to-reach communities] to participate in vaccination. So there’s this institutional barrier towards providing the extra support and care to these communities.
‘If the rebates were appropriate, then we could actually bring on more and more staff and train up more and more people and respond more and more.
‘What gets funded gets done, to be frank.’

The Kimberley region in Western AUstralia has some of the worst Indigenous vaccination rates in the country. (Image: AAP)
Despite the seeming lack of progress in reducing the vaccination rate gap, a Department of Health spokesperson told newsGP vaccinating Aboriginal and Torres Strait Islander people ‘continues to be a priority’ for the Federal Government.
‘To ensure this happens as quickly and effectively as possible, the Government continues to work in partnership with the National Aboriginal and Torres Strait Islander Advisory Group on COVID-19 [which is co-chaired with NACCHO], Aboriginal Community Controlled Health Services [ACCHS], state and territory governments, and individual communities to identify and address specific needs,’ the spokesperson said.
‘The [National COVID Vaccine] Taskforce is also working with the Advisory group and communities across Australia to identify additional ways in which the Government can provide support to ensure that every Aboriginal and Torres Strait Islander has the opportunity to receive COVID-19 vaccines.
‘Additionally, to counter vaccine hesitancy and misinformation, the Taskforce has developed specific communications materials and public relation initiatives.’
The spokesperson also said the Taskforce has facilitated:
- first dose, second dose, booster and 5–11 vaccination clinics in the 30 LGAs and communities of focus
- activating community engagement teams in the 30 LGAs and communities of focus
- providing a significant increase in supply to ACCHS nationally to vaccinate communities
- additional workforce supports and partnerships.
Of the
more than $8 billion spent on the vaccine rollout to date, $29.4 million has been provided to NACCHO and member organisations to support pandemic preparedness, response and vaccine rollout Aboriginal and Torres Strait Islander communities.
Log in below to join the conversation.
Aboriginal and Torres Strait Islander health COVID-19 Omicron vaccine rollout
newsGP weekly poll
Within general practice, do you think there are barriers to providing flu vaccinations? If so, what are they?