News
GPs to receive DoH letter aimed at cutting use of psychotropic medications
The Department of Health wants to reduce psychotropics in aged care – but GPs already know the drugs are not a first line treatment for dementia, according to the RACGP President.
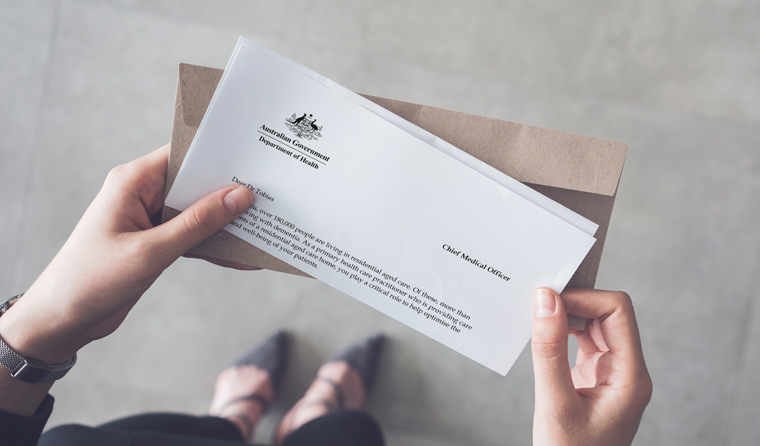 The letter adopts a more muted tone than last year’s opioid warning letter.
The letter adopts a more muted tone than last year’s opioid warning letter.
More than 28,000 health practitioners – mostly GPs – who prescribe in residential aged care facilities (RACFs) will be sent a Department of Health (DoH) letter aimed at cutting inappropriate use of psychotropic medications.
The letter adopts a more muted tone compared to last year’s DoH letter, which warned GPs about opioid use by comparing prescribing habits to a peer average.
However, a smaller group of prescribing practitioners is expected to receive a follow-up letter in 2020 to ‘assist them to reflect on their prescribing patterns of antipsychotics and benzodiazepines’, according to the new psychotropic letter.
The 2018 opioid letter sparked strong pushback among GPs and led to Australia’s Chief Medical Officer, Professor Brendan Murphy, issuing a clarification in newsGP.
In the latest letter, Professor Murphy outlines the fact there has been ‘heightened concern’ over the use of psychotropic medications, such as antipsychotics and benzodiazepines, to manage the behaviours and psychological symptoms of dementia for people living in RACFs.
‘This has been reinforced by the Royal Commission into Aged Care Quality and Safety,’ he wrote.
But RACGP President Dr Harry Nespolon told newsGP that GPs are already aware psychotropic medications are not a first line treatment.
‘GPs know that chemical restraints in aged care facilities are the last resort. Those aren’t my words, they’re what GPs who work in these facilities every day have told me,’ he said.
‘While there has been significant attention on this practice in the wake of the Royal Commission, it’s important to note that chemical restraint is not the norm – it is rare.’
The DoH psychotropic letter adopts a notably different tone to the opioid letter.
‘You would be aware that best practice for managing the behaviours and psychological symptoms of dementia uses a person-centred approach,’ it states.
‘Psychotropic medications are not first line therapy and should only be considered when person‑centred approaches have been maximised and an older person remains distressed, and then only with informed consent of the person or their representative.’
The letter stresses that antipsychotic and benzodiazepine medications are clinically appropriate for pre-existing mental illness and ‘some symptoms’ of dementia, such as hallucinations or anxiety.
‘[M]edications should be trialled for specific symptoms with the aim of reducing and ceasing them as soon as possible,’ it states.
‘These medications do not address many behaviours of dementia, such as inappropriate verbalisation, intrusive behaviours or so-called “wandering”.’
The letter states that these medications may cause harms such as increased confusion, loss of independence, loss of ability to interact, as well as higher risks of respiratory issues, stroke and death.
‘Please know that we are also working with aged care providers, pharmacists and families to reduce usage of psychotropic medications and to maximise person-centred care approaches,’ the letter states.
GPs concerned after receiving the letter can email the DoH team. A dedicated resource page is expected to be available next week.
The letter also recommends Dementia Support Australia and the Dementia Training Program.
Log in below to join the conversation.
aged care chemical restraint psychotropic medication royal commission
newsGP weekly poll
Which of the following areas are you more likely to discuss during a routine consultation?