News
RACGP and ACRRM vow to collaborate on general practice training
A new joint communique has outlined the cooperative approach they will take ahead of the transition to college-led training.
 The approach means RTO contracts have been extended for one year until the start of semester one 2023.
The approach means RTO contracts have been extended for one year until the start of semester one 2023.
The release reaffirms that the Federal Government is also committed to reforming the Australian General Practice Training (AGPT) model, which will see the colleges become directly responsible for training registrars.
RACGP Acting President Associate Professor Ayman Shenouda said the colleges are committed to making general practice and rural generalist training the ‘career pathway of choice’ for prospective students.
‘The return of general practice training to the RACGP provides a unique opportunity to drive further excellence in general practice training, and align it to workforce-distribution strategies that satisfy the healthcare needs of the diverse communities we serve,’ he said.
‘This is a complex and multifaceted set of reforms that will require extensive consultation and collaboration with all of our stakeholders.
‘To allow enough time for the necessary consultation and collaboration, the Minister for Health [Greg Hunt] has offered to extend the regional training organisations’ [RTOs] current contracts for one year until the start of semester one 2023.’
Australian College of Rural and Remote Medicine (ACRRM) President Dr Ewen McPhee ‘welcomed’ the RTOs’ contract extensions and said he does not anticipate reforms will result in any changes to the curriculum, requirements for supervisors or assessments.
‘Importantly, the commitment to transition of AGPT to college-led training arrangements remains on track for 2022, and supporting policy reforms will be considered in a staged approach,’ he said.
‘All parties have agreed to work together to create improvements for GP training, including increasing the attractiveness of [rural generalist] and GP training, improving recognition of supervisors and better aligning training with workforce strategies.’
The joint communique states the RACGP and ACRRM are considering the best approaches to deliver workforce planning and distribution support for the colleges, practices and other settings involved in training GPs, along with the communities that benefit from health services delivered during training and beyond.
It also confirms that the Government is committed to preserving all funding under AGPT in an effort to enhance the general practice training experience.
Part of the joint commitment relates to a shared understanding that Aboriginal and Torres Strait Islander health training remains ‘central’ to transition planning. It confirms that the Strategic Plans Program allocation of $9 million and $27 million salary support funding will continue, and that there will be ongoing engagement with key partners such as the Australian Indigenous Doctors Association and the National Aboriginal Community Controlled Health Organisations to help build stronger outcomes as part of the transition.
‘Earlier this year, the colleges and the Department [of Health] successfully transitioned the administration of the AGPT Program policies and selection functions. This was completed with minimal disruption in readiness for the March 2020 registrar intake,’ the communique states.
‘Planning is underway to ensure future transitions of functions and activities are as smooth as possible as we continue a phased transition approach.
‘The RTOs will continue to provide important education, support and mentoring to their registrars and supervisors whilst they are engaged to do so and we map how we will enhance the next stage of the AGPT.’
As part of the transition, the Government is reportedly ‘keen’ to examine how general practice training intersects with key health strategies under development and workforce planning across multiple rural workforce and training programs, resulting in ongoing discussions with both the colleges.
‘Once we have a common approach, the Department [of Health] and colleges will resume consultations with broader GP training stakeholders about potential reforms and timing of implementation of reforms through the transition,’ the communique states.
‘We are acutely aware that we need to support the current registrars and supervisors over the next few years and we will work together to ensure that change is managed in a way that reduces the impact on registrars and supervisors.’
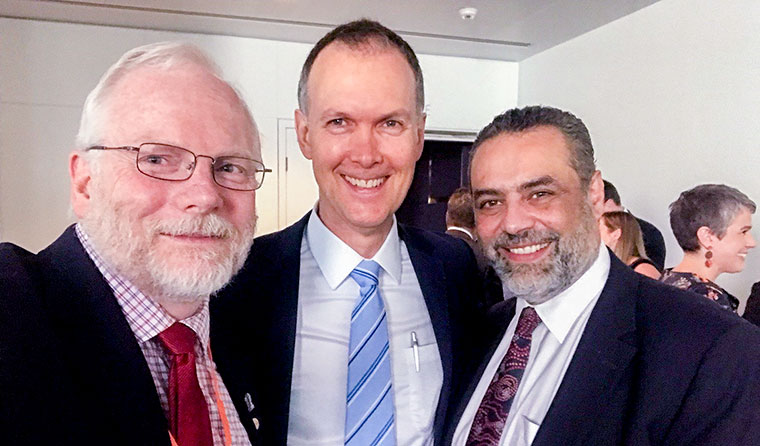 ACRRM President Dr Ewen McPhee, inaugural National Rural Health Commissioner Professor Paul Worley, and Acting RACGP President Associate Professor Ayman Shenouda.
ACRRM President Dr Ewen McPhee, inaugural National Rural Health Commissioner Professor Paul Worley, and Acting RACGP President Associate Professor Ayman Shenouda.
According to the communique, a key issue raised during consultations is that quality ‘on the ground’ experience in practices, supplemented by strong educational resources and educators, is essential.
As a result, the Department of Health and the colleges will work towards improving support and incentives to registrars and their supervisors.
‘We recognise that supervisors may be supervising a range of learners – medical students through to final-year registrars and want to ensure appropriate and enhanced support and resources are available for vertically integrated, quality supervision,’ the joint release states.
‘Collectively, we would like to examine how we can improve financial support to supervisors, better recognise the impact that quality training can have on practice income, and incentivise high quality GP training placements.
‘We would [also] like to make GP training a more attractive proposition for junior doctors to consider. As part of this we are considering options to make registrar conditions better aligned to their hospital based counterparts.’
Two pilot models – one in the Murrumbidgee River that allows registrars to move between the hospital and community primary care while being paid a salary by the Local Health District; and another through the Remote Vocational Training Scheme that tests wage equalisation through subsidising a registrars salary in early stages of training – are currently being tested to further these aims.
‘The Department [of Health] would like to test AGPT models that could provide greater parity for GP registrars and make choosing general practice easier for our junior doctors. This would include exploring salaried models and models that enable portability of entitlements through training,’ the communique states.
‘We need to ensure that we have the right policy and funding settings to achieve the critical workforce distribution objectives of the AGPT, as well as other public investments in medical and health professional training and service learning programs.’
Log in below to join the conversation.
AGPT general practice training RACGP
newsGP weekly poll
Which of the following areas are you more likely to discuss during a routine consultation?