News
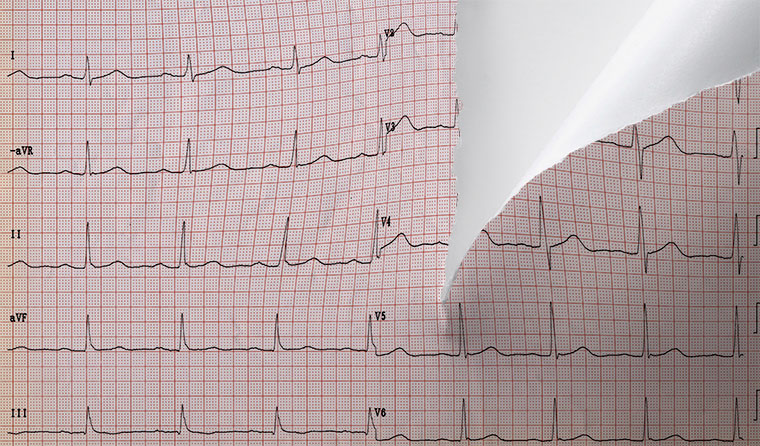
‘Kicking the can down the road’: ECG decision under fire
The RACGP is calling on the Government to abandon another review of ECG items and reverse a Medicare rebate cut.
 A key recommendation from the independent inquiry’s report is restoring the MBS item for ‘tracing and reporting’ of ECGs in general practice.
A key recommendation from the independent inquiry’s report is restoring the MBS item for ‘tracing and reporting’ of ECGs in general practice.
The Federal Government has rejected a key recommendation from the Electrocardiogram Review Committee to reverse a Medicare rebate cut for electrocardiogram (ECG) services.
Instead it announced a further review via the MBS Reviews Advisory Committee once more data is available.
RACGP President Professor Karen Price said she is ‘deeply disappointed’ by the decision.
‘The independent inquiry commissioned by Health Minister Greg Hunt tells us everything we need to know,’ she said.
‘The report clearly states that [patient out-of-pocket costs] may translate in the long term to poorer health outcomes. Conducting another review is just kicking the can down the road.
‘The Government should immediately reverse the Medicare ECG rebate cuts and enable GPs to get on with the job of helping patients at risk of serious heart problems.
‘ECGs save lives and there is no point in reducing patient rebates for these services in general practice.’
The Electrocardiogram Review Committee’s report was published last week. It considered the impact of the August 2020 decision to remove patient rebates for ECG services provided by GPs that included reporting.
That decision meant the previous Medicare benefit of $27.45 for the ECG ‘trace and report’ in a clinic (item number 11700) was reduced to $16.15 under item number 11707.
The item description required it to be for a ‘trace only’ with no report.
This decision was slammed by GPs, and the RACGP warned that the changes to MBS items for ECGs would effectively restrict these services to non-GP specialists and consultant physicians.
In a submission to the committee in April last year, the college argued the changes could compromise patient access to timely diagnosis and management of heart conditions, and called for the restoration of tracing and reporting item numbers.
Following the Federal Government decision this month to wait for more data, the RACGP called for the Government to ‘act decisively’.
‘The Government must properly recognise the valuable work GPs do with ECGs and appreciate how important these services are for patient care,’ Professor Price said.
‘They have got this one wrong; we should be investing in general practice so that GPs can take on services like this that save lives and keep patients out of the hospital system.’
Professor Price said the 2020 changes to ECG items failed to recognise the time required by GPs to interpret ECGs and record the results.
‘Since August 2020, patients are only eligible for a Medicare item for ECG tracing in general practice and are not able to claim for tracing and reporting,’ she said.
‘This is despite the fact that GPs perform interpretation, report results in our patient records and determine what needs to happen next without needing to refer to another specialist for interpretation and reporting.
‘What this means in practice is that patients have to access ECGs via more expensive non-GP specialists and therefore face higher out-of-pocket costs – something that is often completely unnecessary.’
The ECG Review Committee report found there was an immediate 9% reduction in Medicare claims under the new system when compared with the previous 12 months.
The fee for the original tracing and reporting item ‘more accurately reflected the cost of providing this service’, the report states.
It also reported that out-of-pocket payments for ECGs increased $3.91 on average compared to the previous 12 months and were $4.61 higher than the same period 24 months earlier.
The committee also recommended:
- ensuring access for all medical practitioners to the trace and clinical note item (11714) with an increase to the daily number of services claimable
- introducing a new item or amending existing ECG trace and report item 11704 for specialist/consultant physicians to access a trace and report item, which can be claimed with a consultation item
- implementing a fee structure based on the application of a clinical value tier structure.
A Department of Health (DoH) spokesperson said the inquiry identifies ‘challenges distinguishing a single cause of the decline in ECGs’, including COVID-19 disruptions and the expansion of Medicare-funded telehealth.
It said the decision to carry out a second review after another 12 months of data becomes available would ‘allow claiming patterns to settle from the impacts of COVID-19’.
Log in below to join the conversation.
cardiac imaging ECG electrocardiogram MBS Medicare rebates
newsGP weekly poll
Within general practice, do you think there are barriers to providing flu vaccinations? If so, what are they?