News
RACGP calls for changes after ECG Medicare cuts
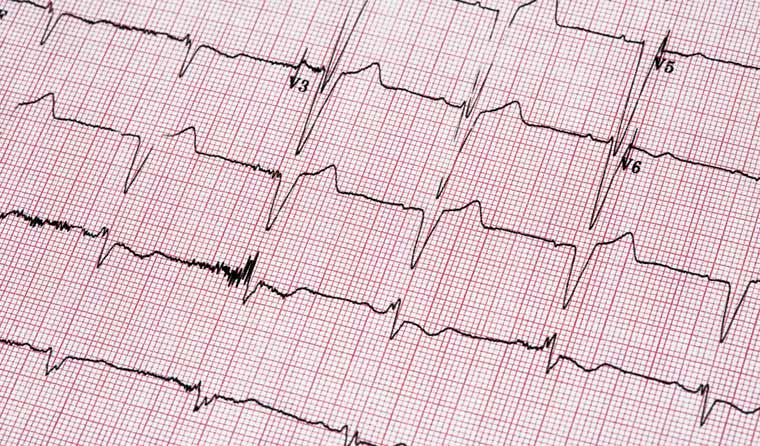
The college wants GPs to be treated for what they are – medical specialists – when billing for electrocardiograms.
 Doctors say the cuts can ‘threaten patient access to timely diagnosis and management of heart conditions’.
Doctors say the cuts can ‘threaten patient access to timely diagnosis and management of heart conditions’.
GPs want fresh changes following last year’s controversial cuts to electrocardiogram (ECG) funding, which doctors say can ‘threaten patient access to timely diagnosis and management of heart conditions’.
The RACGP has put forward a series of recommendations to the Department of Health’s (DoH) Medicare Benefits Schedule (MBS) review for ECGs, arguing for the continuation of tracing and reporting item numbers.
RACGP President Dr Karen Price says the item number 11714 should be used to support access to ECGs conducted by GPs, as well as other specialists.
‘GPs are medical specialists, and it is the RACGP’s position that GPs should be paid the same as other medical specialists for doing the same work,’ she said. ‘This reflects current usual practice.
‘This is particularly relevant in rural and remote areas, where a GP may be the only provider offering a particular service.’
Last August, the DoH introduced changes to the MBS that meant GPs were no longer able to access three item numbers for ECG tracing and reporting. They can request the item numbers accompanied by a referral to the specialist or consultant physician.
The previous Medicare benefit of $27.45 for the ECG trace and report in a clinic (item number 11700) was reduced to $16.15 under the item number 11707. But the description of the number also requires it to be for a trace only, with no report.
The changes – part of the five-year overall MBS review taskforce to overhaul the healthcare funding system – were introduced following a review of cardiac imaging services. In its 2018 review, the Cardiac Services Clinical Committee recommended changing the descriptors of 11700 to 11703, but did not recommend the new item number.
There was strong criticism from working GPs when the ECG changes were announced, who argued they misunderstood or devalued their role.
Dr Atef Asham, Chair of RACGP Specific Interests Cardiology, says the ‘erosion of GP ECG interpretation skills’ left doctors feeling ‘undervalued as primary care specialists’.
‘[This ultimately resulted] in GPs being more reluctant to offer ECG services in their practices and patients being referred to hospitals or secondary facilities to have this service performed,’ he told newsGP.
‘This results in delay in diagnosis and increased inconvenience to patients, as well as fragmentation of care.
‘This is an important issue for GPs who are already under significant financial and emotional stress due to COVID.’
A DoH spokesperson told newsGP the review would be complete by June this year, with a final report to be delivered as soon as possible.
‘Any change to the MBS is a decision for Government,’ the spokesperson said.
In the meantime, Dr Asham says the reduction in fees for the item numbers has made it not economically feasible for many practices to perform ECGs; however, the recommended changes would enable increased service provision once again.
In its new submission, the RACGP argues item number 11714 be amended to ‘twelve-lead electrocardiography, trace and clinical note, by a medical practitioner’, instead of ‘by a specialist or consultant physician’.
‘The rebate for item 11714 [$21.25] is still significantly lower than the rebate for item 11700 [$27.45]; however, it reduces the financial impact on patients receiving this service, and consequently the timely access to ECGs for diagnosis and appropriate management,’ Dr Price said.
‘GPs are specialists in their own rights who have trained for years, and not merely conduits for referral of patients to other specialists. GPs are skilled at conducting, interpreting and reporting on ECGs.
‘Having developed this skill, GPs are saving the health system a considerable amount of cost by providing this service directly to patients and responding to issues in a timely manner.’
Dr Price also says last year’s changes increase out-of-pocket costs and access for patients, place additional demands on hospital departments, and risk later detection of heart disease. She says the total theoretical reduction in benefits to patients from the changes since August 2020 is nearly $5.4 million, given an average of 79,000 services are performed each month.
‘This is a significant increase in out-of-pocket costs at a time when per person personal health spending has increased on average 3.4% over the last decade,’ she said.
‘It is likely that reduced access to ECG tracing and interpretation due to excessive costs will increase demand to hospital departments or result in a lack of early detection of heart disease.’
Dr Price also pointed to the disproportionately high rates of cardiovascular disease among Aboriginal and Torres Strait Islander people and health services, which are absorbing the costs.
The DoH has previously said item number 11707 provides for an ECG trace and interpretation by a GP and ‘more clearly delineates the important roles of GPs and specialists, focused on providing high-value patient-centred care’.
They said a GP consultation could be co-claimed with the ECG.
Log in below to join the conversation.
ECG electrocardiogram MBS
newsGP weekly poll
Health practitioners found guilty of sexual misconduct will soon have the finding permanently recorded on their public register record. Do you support this change?