General practice, the government asserts,1 is at the centre of the health system. Most general practitioners (GPs) agree they have a key role in maintaining the health of the community and viability of the health system at large. However, many also feel that, despite emerging policy initiatives, much of their work is regarded as occurring at the margin, because ‘real medicine’, meaning ‘proper management of diseases’, occurs in the super/specialised hospital domain. Recent Productivity Commission reports emphasised how such sentiments have an impact on maintaining the GP workforce.1,2 These reports highlighted two concerns (Supplementary Tables 1, 2, available online only):
-
the profession’s resilience to cope with the uncertainties inherent in early disease presentations and complexities typical of patients affected by multiple morbidities
-
the profession’s ability to meet various stakeholders’ desired health and/or administrative outcomes.
In this paper, we explore the nature of the work of general practice and how that work affects people and their health outcomes and experiences. We highlight the systemic nature and contextual interdependencies between needs of patients and our ability to meet those needs in different practice contexts. On the basis of these insights, we elaborate that modelling the systemic nature of general practice work can enhance the profession’s input into practice and system redesign in collaboration with local meso-level organisations that support its implementation. Systemic thinking provides the blueprint to achieving a more effective, efficient and equitable health system.
Key features of complex adaptive systems
A complex adaptive system (CAS) consists of many interconnected agents and drivers that influence each other in various ways in different contexts. Changing agents and/or drivers results in feedback that may or may not improve intended system behaviour and outcomes. For example, consultation length is not merely a reflection of disease burden but also of local GP workforce size and nursing and allied health availability. A CAS often shows hierarchical layers that influence each other; for example, GPs interact at the same layer with other primary care services, but their work is also dependent on other system levels, such as local hospital/specialist performance and/or government policies.
General practice in the hierarchy of a complex adaptive health system
Issues affecting GP work and workforce are complex and dynamic, as they are linked and distributed across different organisational levels and varied environmental contexts. They occur in hierarchical systems where higher levels (eg federal health policy and funding) provide contextual constraints that limit the emergence of possible desired and/or undesired outcomes arising from lower levels (eg clinical environment or consultation length).3 General practice, as an institution, resides in the middle of the health system hierarchy (Figure 1). It is especially vulnerable to policy constraints that alter the ability of people and communities to respond to health challenges.
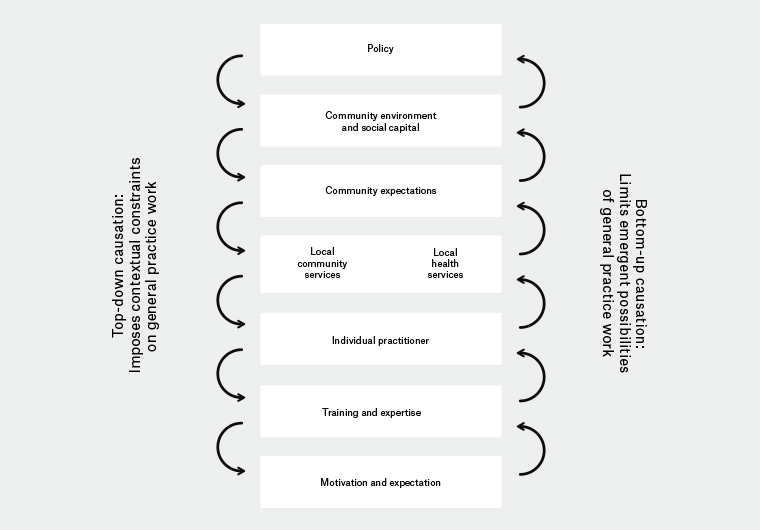
Figure 1. Top-down and bottom-up ‘causal’ relationships affecting general practice work and workforce
The interdependencies of service delivery arise from three areas: patient demands, provider supply and quality-of-care outcomes.
Issues that have an impact on effective, efficient and equitable care delivery in general practice include:
-
socioeconomic determinants
-
patient expectations, demands and needs
-
healthcare system demands and quality/outcome expectations
-
GP/GP team workforce numbers, composition and distribution
-
general practice financing
-
interdependencies with institutions, including primary health networks, public and private hospitals, and community health and social services.
Influence diagrams illustrate the interdependencies between the competing interests inherent in a CAS (Figure 2). They are powerful system tools to achieve a shared understanding about the nature of complex problems and facilitate the emergence of mutually acceptable solutions.
.jpg.aspx)
Figure 2. Influence diagram of general practice care
GP, general practitioner; SES, socioeconomic status
The interdependencies of service delivery arise from three areas: patient demands, provider supply and quality-of-care outcomes. The diagram highlights that not all factors influencing service delivery are under the control of the profession itself – the total general practice workforce depends on policies of student intake, interest in general practice training and the status and relative remuneration differential within the health professions.
The influence diagram reveals three major dynamic feedback loops, two with an additional branching loop:
- Service delivery influences patient care need perceptions and generates patient demand and expectations. The level of actual demand determines the average workload; workload has an impact on practitioners’ attitudes and expectations, which affect – contingent on local circumstances – the length of consultations, which in turn has an impact on service delivery.
- Another branch of this loop entails the impact of service delivery on the quality-of-care and patient-related outcomes, which in turn has an additional impact on patient care needs and perceptions.
- Service delivery affects costs, which modulate patient care need perceptions and patient service demand and expectations, which affect – contingent on local circumstances – the length of consultations, which in turn affects service delivery.
- Service delivery uses available technology, which influences costs and in turn affects service delivery.
- Another branch of this loop entails that costs influence patient care need perceptions and modulate patient service demand and expectations. The level of actual demand determines the average workload; workload has an impact on practitioners’ attitudes and expectations, which affects – contingent on local circumstances – the length of consultations, which in turn has an impact on service delivery.
Each variable potentially represents a subsystem with its own dynamics. For example, the ‘cost’ variable can entail different remuneration models (fee-for-service, capitation, salary), and the ‘service delivery’ variable can entail different service delivery models (acute care, chronic disease management, medical home). The importance here is to appreciate that subsystem changes have a global impact on the system of interest.
Note: Influence diagrams are simplified representations of the real world and only contain those variables agreed to have an impact on the function of the system.
General practice work – consultations are central
In general, health profiles have been unchanged for more than 50 years – 80% of all people feel healthy or at least healthy enough not to seek health professional care at any time.4–6 Equally, most primary care consultations result in non-specific diagnoses;7–9 that is, most people seeking GP care do so for reasons other than specific diagnosis management (Figure 3). Conversely, the ageing population and rise in multiple morbidities in younger populations have necessitated longer consultations addressing care planning and prevention needs. 10 These ecological features of medical care have important implications for the general practice workforce in terms of numbers, skills and expected care delivery tasks.
The key to ‘good GP care’ is the consultation – the ‘production unit’ of care where the majority of decisions are made about using ‘limited health and social care resources’.11 What is achieved in the consultation affects both the quality of care outcomes and future real and/or perceived care needs. Consultations are influenced by a variety of feedback mechanisms (Figure 2), such as the outcomes they previously achieved and the context in which they occur (eg rural or remote location, socioeconomics, workplace and workforce capacities/capabilities).
.jpg.aspx)
Figure 3. Health in the community: Community epidemiology4 (A) and diagnoses distribution resulting from primary care consultations7 (B)
The ‘ecology of medical care’4 has shown that the Pareto distribution applies to the need for healthcare – 80% of people are healthy or feel healthy enough not to require healthcare; of the remaining 20%, 80% solely require primary care services (16% of the total), of the remaining 20%, 80% require secondary care (3.2% of the total); and the remaining 20% require tertiary care (0.8% of the total). Vice versa, Braun’s studies showed that 80% of all primary consultations result in 20% of all diagnoses (mostly unspecific); the remaining 20% of consultations cover 80% of all diagnoses.7 The key message from these studies is that subjective health/illness experience and objective disease diagnosis often do not coincide – the majority of people who may have symptoms but no or little illness experience rightly do not report to a care provider, but some will ultimately be found to have an identifiable disease, and many people who seek help because of their degree of illness experience ultimately do not have objectively identifiable disease.
Four feedback loops affecting general practice work and its workforce include:
-
patient service demand – influenced by technology, cost of care and perceptions of care need
-
consultation length – influenced by GP attitudes, skills and expectations, local workforce numbers, local socioeconomics and available support services
-
quality of care outcomes – influenced by service delivery and integration of care (both influenced by population characteristics)
-
service delivery – influenced by consultation length, technology, integration models and cost of care.
Service demand
Care needs are influenced by personal, cultural, socioeconomic and disease burden factors. Personal health experience coupled with personal resilience and prior healthcare experiences shape help-seeking demands. Third party promotions such as constant direct-to-consumer advertising of pharmaceuticals and therapeutic technologies (regardless of their real benefits) promote services, whereas rising cost of care dampens actual demand.
Consultation length
Average consultation length is the best available ‘proxy indicator’ of quality of care. Consultation length is influenced by a number of factors, including patient and practitioner attitudes and expectations, and workforce and socioeconomic circumstances. Longer consultations result in better decision making and resource use.12,13 More advantaged patients not only have better access to care, they also have longer consultations and better health outcomes.14 Lower socioeconomic communities attract fewer doctors and have fewer resources, resulting in reduced consultation time, ultimately threatening high-quality care delivery and population health, and increasing the risk of premature mortality.
Quality of care outcomes
Quality of care and health outcomes are a function of actual service delivery and the integration of care between various service providers. Quality is a contested concept;15 while bureaucracy is more interested in quality as measured by disease-based criteria and cost per service, patients attribute greater value to subjective outcomes of the doctor–patient relationship and enablement,16 self-rated health and quality of life.17 Measures like ‘days of enablement to manage chronic pain’ or ‘days of poor self-rated health’ better reflect the dynamics of ‘longitudinal generic general practice care’ than a narrow guideline-driven model of disease care.
Service delivery
The productivity of consultations is primarily a function of their length,11,18 but it also depends on care integration among nursing and allied health professionals, specialists, diagnostic and hospital services, as well as service availability and affordability.
Dynamics affecting general practice work
General practice work is limited by multiple levels in its capacity to deliver effective, efficient and equitable care. While some aspects of general practice work can be modified from within, higher level policy changes are needed to overcome the systemic nature of the perpetuation of the inverse care law; that is, more care is provided to those with better health, while those with greater care needs receive less and/or delayed care.19 For general practice to adopt work practices that overcome the inverse care law, one needs to consider the effects of changes at higher and lower system levels.
Higher level constraints limit what lower levels can achieve
Current policies have delivered inadequate GP numbers in low socioeconomic status communities.1 This reduces the consultation time available to fully understand the nature and context of each person’s illness and disease and the broader care needs. More resources are required to coordinate those needs beyond specific disease care, including collaboration and integration with social support services.
Healthcare financing remains volume-driven, and policies support market philosophies, resulting in increased demand for the latest pharmaceuticals and therapeutic technologies, rapidly increasing cost of care. These factors constrain the equitable provision of ‘right care’, especially to low socioeconomic status patients and communities.
Lower levels can only achieve what is possible within the constraints of higher levels
The effectiveness of general practice consultations depends on continuity of care and the resulting therapeutic relationships that can be impaired by top‑down performance demands in a siloed and resource-constrained environment (limited general practice workforce/support services). 2
Patients’ frustration resulting from ‘poor care’ attributable to resource constraints may delay future care-seeking and thus decrease demand, achieving short-term cost savings. However, unresolved complaints and/or delayed treatments result in more severe disease states associated with more costly care and eventually higher health system costs. ‘Poor care’ ultimately frustrates and increases workload demands. A feedback loop with serious negative consequences drives down general practice recruitment, entrenching substandard care delivery and health outcomes, and lowers the communities’ trust and expectations.
Enhancing practice and local health district capacities and capabilities
As discussed, higher system levels influence lower level functions, and Australia’s jurisdictional divide has long increased the potential for functional complexity and conflict. However, signs of emerging national consensus bring hope that CAS principles may yet emerge to guide necessary health system reform. The critical messages common to both levels of government relate to (Table 1):
-
care being patient-centred, continuing and coordinated
-
fragmented health silos giving way to regional-to-local integration via differing local models
-
decision-making responsibilities and resources delegated to meso-level organisations working with local communities and providers to deliver what is needed while building quality, capability and connectedness
-
health financing moving from remunerating volume to recognising and incentivising value – specifically improved quality and outcomes.
|
Table 1. Differing demands – Can we reconcile the ‘dichotomy’ of top-down policy demands with the bottom-up nature of general practice work?
|
|
Political challenges
|
-
Ensuring the role of general practice as the providers of first contact, longitudinal generalists, medical care gatekeepers and coordinators
-
Coping with ageing and the rise in multimorbidity
-
Embracing medical homes
-
Ensuring that Local Area Health Networks coordinate the entire care needs of their population
-
Ensuring person-centred care in an environment of ‘mega centres’
-
Reconciling remuneration demands while sustaining funding to the health system as a whole
-
Sustaining new care delivery models beyond their incentive-driven initiation phase
|
|
The nature of general practice work
|
-
Providing person-centred healthcare where the patient’s needs, values and desired health outcomes always remain central to the general practitioner’s evaluation and management processes
-
Facilitating continuity of care through the continuing patient–doctor relationship and knowledge of the patient, and coordination of clinical teamwork, resources and services
-
Providing comprehensive care, spanning prevention, health promotion, early intervention and the management of acute, chronic and complex conditions
-
Providing whole-person care by addressing the interplay between biological, psychological and social contributors to health
-
Applying diagnostic and therapeutic skill to manage uncertainty, undifferentiated illness and complexity, and applying best-practice evidence in the light of individual circumstances
-
Promoting coordination and clinical teamwork to deliver accessible, integrated patient care: leading, supporting and coordinating flexibly configured clinical teams and engaging with diverse specialists and other sector services according to individual patient or family needs
|
Modelling general practice work and workforce
The CAS framework discussed above provides the basis for collaborative design of system models to explore potential changes to GP work and workforce. Redesign efforts applied to the hierarchical nested CAS can now be successfully managed using emerging data analytics to support a mix of qualitative and quantitative modelling of ‘big data’. Modelling specifically allows even counterintuitive solutions to be evaluated in a safe environment; it ultimately helps to find the ‘most likely best solution’ to improve care delivery in the real world. Modelling can answer questions like:
-
How do remuneration models (fee-for-service, capitation, ‘bundling’, pay-for-performance, salary) affect workload, service delivery, quality of care and cost?
-
Is the medical home-style service delivery model scalable and does it result in greater equity, higher quality and greater cost-effectiveness of care?20,21
-
Can technology – particularly at patient and primary care level – really improve healthcare and health outcomes?
-
Does patient illness monitoring and team care reduce healthcare usage and improve patients’ quality of life?22
Models can take into account different geographic and socioeconomic settings, different practice configurations, different provider attributes and attitudes, and various levels of resource allocation and remuneration frameworks to identify which desired outcomes are most likely achievable, and which unintended consequences may emerge (eg gaming the system and thus disadvantaging some patient groups).
Modelling to reach consensus
Modelling of small changes to health experiences, health seeking and service provision has shown an impact on general practice work and healthcare costs.23 Current growth in service and resource use may make the health system quickly unsustainable. Significant savings are possible from reducing service and resource demands.
This example highlights how modelling could be used to facilitate a necessary discourse between practitioners and bureaucrats who, on face value, see very different opportunities in such findings.23 Divergence challenges the status quo; shared understandings are needed to develop an accountability framework that harmonises accountability across clinical and managerial domains – improving effective and equitable service delivery and health outcomes efficiently.
Conclusions
Understanding the work of general practice and the challenges to its workforce can only be fully appreciated within a CAS framework. This demands the deconstruction of limiting (largely economically driven) meta-concepts of demand, supply and quality. A CAS model more clearly explains the interconnected and interdependent nature of the discipline at the centre of the health system.
The complexities of general practice work and the impact on its workforce can be ‘easily’ understood. However, evaluating the potential dynamic benefits and risks of change and redesign is challenging and best assessed by continuous qualitative and quantitative modelling. Modelling results in system-wide evaluations of ‘political, economic and/or service model dogma’.24
To fulfil its remit of meeting each person’s care needs in their community, general practice ultimately must have the right workforce numbers with a distribution to match a communities’ needs, backed by the right kind of support services and financial resourcing. Only then will the profession be able to exercise its capabilities to maintain population health in the most effective, efficient and equitable way.25
Key points
-
GPs need to engage in the development of dynamic system models that allow the ongoing evaluation of changing disease burden, socioeconomic conditions and policy settings on their work, workforce and practice configurations.
-
The consultation is the main ‘production unit’ of care where decisions are made about the use of ‘limited health and social care resources’.11 Understanding a patient’s illness experience and care needs entails sufficient time, continuity of care and the right support services.
-
Meeting each community’s care needs requires a general practice workforce with the right capabilities, numbers, distribution, support systems and financing arrangements.
-
General practice needs to engage with local meso-level organisations that provide essential support for practitioners and practices to implement best adaptive care redesign commensurate with its population needs.
-
In areas of socioeconomic and health disadvantage, the inverse care law still applies, with general practices likely to require higher levels of practice, workforce and financial support.
|
Supplementary table 1. Key issues affecting general practice and the provision of healthcare as identified by the Productivity Commission in 2005
|
|
Australia's health workforce – 20051
|
|
The context for future workforce policy
-
Changed mix of disease burdens
-
Timely access to high-quality health services
-
Technological change will continue to be an important contributor to growing demand
-
Ageing population will increase demand
-
The average age of health workers is increasing
-
Impact on spending by 2044–45 – minimum of 16% of gross domestic product (GDP; government outlay of 10% of GDP)
|
|
Strategies for achieving improved health workforce outcomes
-
Reduction in demand for healthcare through wellness and preventive strategies
-
Short-term increases in education and training – but time delay
-
Focus on retention and re-entry
-
Responsiveness to changing needs and pressures
|
|
Address systemic impediments in workplace arrangements that reduce efficiency, effectiveness and responsiveness
-
Fragmentation of responsibilities
-
Coordination is not always effective
-
Rigid regulatory arrangements
-
Funding and payment arrangements detract from efficient outcomes
-
Entrenched workplace behaviours
|
|
An integrated reform program is proposed
-
Maintain the provision of high-quality and safe healthcare
-
Adopt a whole-of-workforce perspective
-
Recognise the interdependencies between the different elements of health workforce arrangements and ensure that they are properly coordinated
-
Establish effective governance arrangements
-
Ensure that services are delivered by staff with the most cost-effective training and qualifications to provide safe, quality care
|
|
Modifying funding and payment mechanisms to improve incentives
-
Implement a more transparently objective process for assessing proposed changes to: the range of services and health professionals; referral rights for diagnostic and specialist services; and prescribing rights under the Pharmaceutical Benefits Scheme according to their safety, efficiency and cost-effectiveness
-
Investigate the extent of the bias in rebates in favour of procedural over consultative services
-
Introduce Medicare Benefits Schedule rebates payable for a wider range of services delegated by an approved practitione
|
|
Other issues
-
Projecting future workforce needs
-
General practice after-hours services near hospitals
-
Medical indemnity arrangements
-
Taxation and superannuation policies
|
|
Source: Productivity Commission. Australia's health workforce. Productivity Commission Research Report. Canberra: Productivity Commission 2005.
|
|
Supplementary table 2. Key issues affecting general practice and the provision of healthcare as identified by the Productivity Commission in 2017
|
|
Shifting the dial – 20172
|
|
Integrated care
-
New regionally located care model offering funding and fostering attitude changes
-
Regional alliances between Local Hospital Networks, Primary Health Networks and others
-
Move retail pharmacy into an integrated care system
-
Use information effectively
|
|
Patient-centred care
-
Develop Patient Reported Experience and Outcome Measures and publish
-
Use My Health Record to improve information flows to patients and increase health literacy
-
Identify and focus on high users of system
|
|
Funding for health
-
Funding pools for Local Hospital Networks and Primary Health Networks to use for preventative care and management of chronic conditions at the regional level
-
Provide greater autonomy to allow regional solutions
|
|
Quality of health
-
Require fast-track assessment of low-value care identified by overseas agencies
-
Educate clinicians and measure and divulge their use of low-value procedures
-
Improve patient literacy
-
Defund demonstrably low-value procedures
-
Remove subsidies for ancillaries in private health insurance
|
|
Using information effectively
-
Follow recommendations of the Commission’s 2017 inquiry into Data Availability and Use
-
Adoption of eHealth throughout the health system
-
Disseminate best practice through existing agencies
|
|
Source: Productivity Commission. Shifting the dial: 5 year productivity review. Report no. 84. Canberra: Productivity Commission, 2017; p. 43
|