This article is the first in a two-part series on the management of hernias.
Groin hernias are common in general practice and most cases are symptomatic. While definitive treatment is surgical, general practitioners (GPs) need a working knowledge of all aspects of this condition because of their integral role in the patient’s journey. When referring a patient, GPs should be aware of useful information to be obtained from history, examination and medical imaging. GPs should also know the basics of surgical treatments, to interpret discharge letters and provide preliminary counselling to patients before referral. Equally important is an understanding of postoperative care and complications, as GPs are often the point of first contact following discharge.
Anatomy
A hernia is the protrusion of a viscus beyond the cavity in which it is normally contained. Viscera herniating through the abdominal wall typically do so within a potential space known as the hernia sac, which is lined by the peritoneum. Unlike its contents, the sac is fixed and cannot reduce into the abdominal cavity. The inguinal region or groin is the lowermost part of the abdominal wall. Its anatomy offers three potential hernia defects (Figure 1).
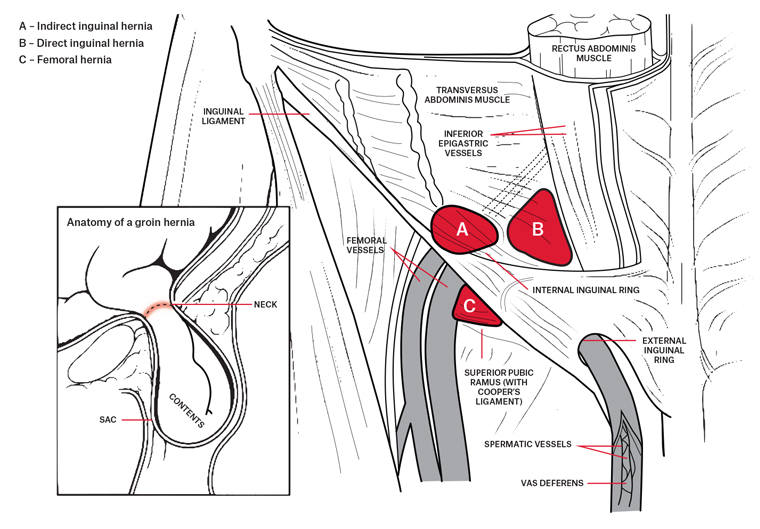
Figure 1. Types of groin hernia: anterior view
Indirect inguinal hernias arise from the deep inguinal ring, through which remnants of a persistent processus vaginalis (the hernia sac) may extend for a variable length down the inguinal canal. The inguinal canal also contains spermatic cord structures in males and the uterine round ligament in females. Patency of the processus may extend as far as the scrotum (inguinoscrotal hernia). Although indirect inguinal hernias result from a congenital defect, they may not manifest clinically until adulthood following progressive dilatation of the deep ring and distension of the hernia sac with intra-abdominal contents.
Direct inguinal hernias arise medial to the deep ring, where the musculo-aponeurotic abdominal wall is most attenuated, and may become further weakened with advancing age and increased intra-abdominal pressure. Congenital defects may also occur here.
Femoral hernias arise from the femoral ring, bounded by the inguinal ligament anteriorly, the femoral vein laterally, the fascia of the pectineus muscle posteriorly and the lacunar ligament medially.
Epidemiology and pathology
Inguinal hernias are up to 10 times more common than femoral hernias and occur predominantly in males.1–3 Femoral hernias are several times more frequent in women.1,2 The incidence of repair of all groin hernia types increases with age.3
Other risk factors for primary groin hernias include family history, chronic obstructive pulmonary disease, smoking, low body mass index, chronically raised intra-abdominal pressure and collagen vascular disease.4,5 Heavy lifting per se is not conclusively associated with groin hernia incidence.6
Strangulation occurs when reduction of hernia contents is impeded by the relative narrowness of the neck of the sac at the level of the abdominal wall defect. Without prompt reduction, restricted venous outflow causes progressive swelling, obstruction of arterial inflow and venous gangrene. If strangulated contents are bowel, perforation and peritonitis may ensue.
Incarceration is an ambiguous term suggesting simple irreducibility or strangulation. To convey the appropriate sense of priority, a hernia is better described as spontaneously reducible, reducible with taxis (and/or with difficulty), irreducible (without strangulation) or strangulated.
Recurrent inguinal hernias are classified separately. They account for 12–13% of all groin hernia repairs7 and can occur at variable times after the initial operation. They are typically direct, caused by an underlying deficiency in the posterior wall of the inguinal canal that may have evolved since the initial surgery or was not adequately repaired at the time. Because of the small size and anatomical boundaries of the hernia defect, femoral hernias rarely if ever recur following repair.
History
Groin swelling
Patients typically describe an intermittent groin swelling, precipitated by physical exertion or increased intra-abdominal pressure and relieved by relaxation, lying supine or local pressure (taxis). Unless a hernia is strangulated, there is usually no pain; the sensation is, rather, a dragging discomfort. For small hernias, the only symptom may be the swelling itself. Symptoms of strangulation are a painful, irreducible groin swelling, possibly associated with symptoms of bowel obstruction (colicky abdominal pain, vomiting, absolute constipation). This would warrant urgent surgical referral.
Acute or chronic groin pain in the absence of localised swelling is unlikely to be a hernia – certainly not one requiring surgical repair – despite an ultrasound report stating ‘patent processus vaginalis containing omental fat’. This may be due to so-called inguinal disruption, which may include osteitis pubis and musculotendinous injuries.8 These patients often require tailored multimodal management.9 If there is any doubt, surgical referral is advisable.
Reducibility
Hernias, particularly large inguinoscrotal ones, may be irreducible without strangulation because of adhesions forming between the visceral contents and hernia sac. This will influence the surgeon’s operative approach.
If a hernia is reducible, it is worth documenting how easily it reduces. Reduction may occur spontaneously after cessation of activity or on lying down. In other cases, taxis is required, because the neck of the sac at the level of the abdominal wall defect is narrow relative to the capacity of the sac itself. Expedited surgical referral is desirable for hernias that are difficult to reduce because of increased risk of strangulation. Similarly, a patient should be given priority if they describe symptoms suggestive of bowel obstruction associated with manifestation of their hernia.
Past history
When considering surgical intervention, a detailed history of active comorbidities, previous surgery and current medications is essential. While chronic conditions, such as diabetes and obesity, may affect overall operative risk and complications, smoking is one modifiable factor directly associated with postoperative recurrence.10 Recurrence following previous hernia repair is itself a risk factor for further recurrence.11 Whether a previous hernia repair was open or laparoscopic may influence the surgeon’s decision regarding subsequent repair technique. Past lower abdominal operations, including open appendectomy, may be a relative contraindication to a totally extra-peritoneal (TEP) laparoscopic repair because of obliteration of the operative plane by adhesions. Finally, special consideration may be required for patients on long-term anti-platelet or anti-coagulant agents.
Assessment
Physical examination
The deep inguinal ring lies midway between the anterior superior iliac spine and the pubic tubercle. An indirect inguinal hernia emerges here to extend downwards and medially along the inguinal canal. Two fingers placed at this site may sense a cough impulse if not already noted on visual inspection. The impulse of a direct inguinal hernia arises medial to the deep ring, while a femoral hernia typically emerges below the inguinal ligament, lateral and inferior to the pubic tubercle. Femoral hernias, when present, are almost always irreducible.
If not elicited in the supine position, a suspected hernia may manifest if the patient lifts their head off the pillow as if to do a sit-up, which increases intra-abdominal pressure. Failing that, adopting a standing position may allow gravity to assist demonstration of hernia prolapse.
Forcible reduction of a painful hernia is contraindicated, as this may be a sign of strangulation with necrotic bowel. Immediate surgical referral is required.
Imaging
No imaging investigations are indicated for a groin hernia evident on clinical examination,7 or where the patient convincingly describes a groin swelling that arises on exertion and subsides with relaxation, lying down or manual compression. However, ultrasonography may be useful in distinguishing an irreducible or strangulated hernia from lymphadenopathy. It may also occasionally be indicated for confirming the diagnosis when physical examination is difficult, such as in patients who are morbidly obese. A recent consensus statement recommends magnetic resonance imaging as the investigation of choice for suspected inguinal disruption or the so-called sportsman’s groin hernia,8 although it is unlikely that this would be considered practicable in the general practice setting.
Treatment
Non-operative management
Watchful waiting can be adopted for clinically evident, minimally symptomatic inguinal hernias, although 75% will require surgery within ten years.12 Clinically evident femoral hernias, even with minimal symptoms, should be referred for surgery, given the higher risk of strangulation.
While orthotic devices can be fitted for patients deemed ineligible for surgery, they are less efficacious in relieving symptoms than operative repair.13,14 Moreover, if a patient is unfit for general anaesthesia, spinal or local anaesthesia is usually feasible for open operations, even on inguinoscrotal hernias.15 Eligibility for operative management or general anaesthesia should only be decided at specialist consultation.
Operative repair
The basic principles of hernia repair are reduction of sac contents, excision of the sac (herniotomy) and repair of the abdominal wall defect (herniorrhaphy). Current best evidence indicates that tension-free repair with prosthetic mesh gives the lowest recurrence rate.7 Open (Lichtenstein) hernia repair, via a groin incision, lays mesh superficial to the transversalis fascia. With laparoscopic repair, mesh is placed deep to the transversalis fascia, either by a trans-abdominal pre-peritoneal (TAPP) or TEP approach. Regarding long-term recurrence, various meta-analyses conclude no significant difference between Lichtenstein, TAPP or TEP operations.16–20
Strangulation is an absolute contraindication to laparoscopic repair. Relative contraindications include irreducible and/or large inguinoscrotal hernias. As with any minimally invasive procedure, patients are advised that conversion to open operation is likely if access is technically compromised.
Femoral hernias follow similar operative principles to inguinal hernias, although because of the small size of femoral canal defect, open repair may not require mesh; approximation of the pectineal fascia to the inguinal ligament with non-absorbable sutures usually suffices. With a laparoscopic approach, mesh is laid over the femoral opening and the posterior wall of the inguinal canal.
Aftercare
Hospital stay
Comorbidities or social circumstances notwithstanding, elective laparoscopic or open repairs can be performed as day surgery. Hospital stay may occasionally be prolonged if urinary catheterisation is required for post-operative retention, typically in older male patients.
Complications
Although it is the surgeon’s responsibility to inform patients of specific operative complications, awareness of these is essential for GPs, to whom patients may initially present when complications arise.
Early postsurgical complications occur with similar frequency for open and laparoscopic procedures: 7–8% for wound seroma or haematoma,21 1% for wound infection,21 0.7% for testicular ischaemia or atrophy22 and less frequently for mesh complications such as erosion, migration or infection.23 While life-threatening complications are extremely rare, laparoscopic repair has a 0.09–0.18% risk of vascular or visceral injury.24 Areas of hypoaesthesia or painful neuroma may occur where cutaneous nerves were injured or divided in gaining access for open repair. Chronic pain affecting daily living is around 2–4%.23
Recurrence is the main late complication. Depending on follow-up duration, rates following primary inguinal hernia repair are up to 15%,25 although actual reoperation rates are usually less.26 Determinants of recurrence are similar to those for primary hernias but also include technical expertise, which is a function of a surgeon’s case volume or specialisation.27
Regarding emergency repairs, overall complications are increased, compared with elective repairs; this is especially true for elderly patients because of increased comorbidities.28 While mortality for elective repairs approaches that of the general population, it is increased several-fold in emergency situations, such as strangulation necessitating bowel resection.29
Resumption of activity
No study has shown that resumption of normal activities earlier than the usually prescribed three to five days increases the risk of recurrence or other complications following elective repair.7 As reasons for delayed recovery mostly relate to pain or wound-related problems,30 most surgeons would offer a laparoscopic operation over an open one unless contraindications exist.
Driving a vehicle merits specific discussion. Common sense should prevail – if reaction time to manipulate foot controls is likely to be slowed as a result of groin pain, a patient should refrain from driving.
Conclusion
- Knowledge of basic groin anatomy facilitates initial assessment of groin hernias.
- History and physical examination determine indications and priority for surgical referral.
- While watchful waiting can be adopted for some inguinal hernias, all cases warrant referral to a surgeon.
- Additional imaging is superfluous if signs and/or symptoms suggest a hernia. Ultrasound can differentiate an irreducible hernia from other lesions.
- Operative repair, by various possible approaches, is feasible in most cases. Serious post-operative complications are relatively uncommon, although technical expertise may influence recurrence rate.
- Post-operative resumption of usual activities should be encouraged as soon as the patient is comfortable.