The prevalence of chronic kidney disease (CKD) in Australia is estimated to be as high as 11%,1 although the rate of undiagnosed CKD is substantial. CKD prevalence is expected to continue to rise as a result of Australia’s ageing population, and the increasing prevalence of diabetes, hypertension and cardiovascular disease, which contribute to susceptibility and disease progression.2 CKD is associated with increased mortality, but is also a significant risk factor for cardiovascular morbidity and mortality.3 The majority of patients with early stage CKD are most appropriately managed in the primary care setting.4 However, if a patient’s CKD deteriorates and referral to a nephrologist is required, timely referral allows consideration of more options for clinical management prior to commencing dialysis or transplantation.5
Globally, it is acknowledged that the nephrology workforce has not increased to meet the rise in nephrology referrals.6 Historically, Australia has lagged behind North America and many European countries in the size of the nephrologist workforce.7 A decade ago, there were significant concerns regarding the size of the future nephrology workforce,8 but there has been rapid expansion of Australian nephrology trainee numbers since then.9 Yet, outside metropolitan areas, a shortage of nephrologists persists in regional, rural and remote Australia.10 The maldistribution of nephrologists affecting rural Australia is exacerbated by the higher prevalence of all chronic disease, inclusive of CKD, particularly end-stage kidney disease (ESKD) in rural Australia,11 along with the higher prevalence of CKD and ESKD among Aboriginal and Torres Strait Islander peoples, who comprise a larger proportion of the rural and remote Australian population.12
Efficient access to specialist nephrology services relies on appropriate referrals and sufficient detail in the referral documents. In Australia, nephrology referral guidelines have been available to assist primary and secondary care providers since the early 2000s.13 These guidelines are founded on the key indicators of estimated glomerular filtration rate (eGFR), proteinuria/albuminuria, renal imaging and blood pressure.13,14 Nephrology referral guidelines provide a framework that can be used in primary care to ensure the right patients are referred to specialist nephrology services at the right time and for the right reasons, after appropriate investigations have been completed. Patient preference is also an important consideration. Patients with CKD may be more appropriately treated conservatively in primary care if they are of advanced age, have slowly declining kidney function, are frail or wish to avoid demanding or costly treatments.15
There is a considerable body of evidence that highlights the benefits of timely referral of appropriate patients from primary care to specialist nephrology services. A systematic review of 40 longitudinal cohort studies found early referral to nephrologists (a minimum of six months prior to initiation of dialysis) to be associated with reduced mortality, hospitalisation, higher uptake of peritoneal dialysis and earlier creation of arteriovenous fistulae for patients with CKD, compared with those referred to nephrologists less than six months before dialysis commencement.5 Another study reported that early referral was further enhanced by frequent (three-monthly) nephrology care in the six months prior to initiating dialysis.16 A study of referrals to tertiary and regional renal services, and to a private practice in Queensland, Australia, found that only 65% of referrals met referral criteria in the first 12 months after the use of eGFR reporting.17 Another study, in metropolitan New South Wales, examined 200 randomly selected nephrology referrals between 2008 and 2011, and found that 25% of referrals did not meet national nephrology referral guidelines.18
The impact of suboptimal referral patterns on the efficient provision of nephrology care is an important consideration in areas of nephrologist workforce shortage, which is typical of much of regional and rural Australia. Optimal referrals ensure that patients with the greatest needs are referred quickly and differentiated from patients most appropriately managed in primary care. The aim of the study was to assess the proportion of CKD referrals to a regional nephrology outpatient service that contained sufficient information to be considered against Australian referral guidelines, and the proportion of patients referred appropriately.
Methods
This study was performed in a regional centre during a time when three nephrologists provided outpatient services. This equated to less than one full‑time nephrologist to service a catchment population of approximately 120,000 people. Ethical approval for the research was granted by Goulburn Valley Health’s Human Ethics and Research Committee (reference number: GVH 04/15).
All new adult referrals to the nephrology clinic lists at Goulburn Valley Health from January 2013 to December 2015 were reviewed by a member of the research team according to the inclusion criteria. Referrals were excluded if the patient failed to attend the nephrology clinic, or if the referral was not for CKD opinion or management. Referrals for follow-up after acute renal injury or for potential renal transplant donor workup were excluded, as were those for patients being transferred from other nephrology services (Figure 1). Referrals were received from general practitioners, other healthcare providers or subsequent to an inpatient episode. Data collected from referral letters included:
- reason for referral
- age
- gender
- postcode
- eGFR
- sequential eGFR
- ultrasound result
- nephrology diagnosis (if known)
- albumin-to-creatinine ratio (ACR)
- protein-to-creatinine ratio (PCR)
- urinary red cells
- haemoglobin
- parathyroid hormone (PTH)
- blood pressure
- anti-hypertensive medication (including angiotensin converting enzyme [ACE] inhibitors, angiotensin receptor blockers, ‘other’ antihypertensive medications, diuretics and statins).
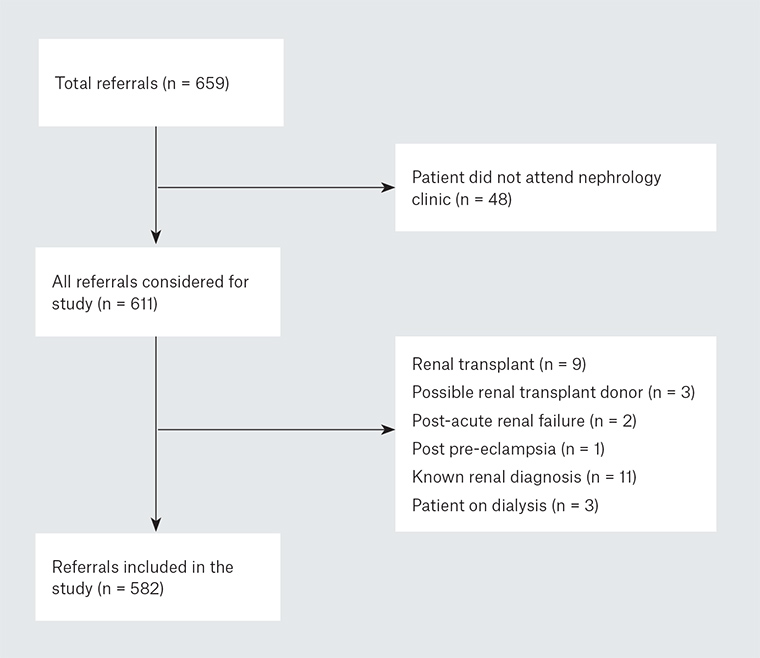
Figure 1. Nephrology referrals excluded from analysis
Additional data collected included other cardiovascular comorbidities (including ischaemic heart disease [IHD], acute coronary syndrome, angina, coronary artery bypass graft, cardiac stenting, cerebral vascular disease [CVD], heart failure [HF], peripheral vascular disease [PVD] and aortic aneurism). A prior history of hypertension was also noted. In addition, eGFR and urinary albumin-to-creatinine ratio (ACR) or protein-to-creatinine ratio (PCR) results from tests undertaken at the time of first attendance at the renal clinic were collected.
All eGFR and urinalysis data from the referral letters were compared to the guidelines for recommended referral to nephrology services as detailed in Kidney Health Australia’s Caring for Australasians with renal impairment (KHA-CARI) guidelines for CKD,14 and assessed as meeting the guidelines or otherwise by the research team.
Statistics
For analysis, data were entered into SPSS version 21 and descriptive analysis performed. Descriptive data are presented as mean (range) and as a percentage of all referrals where appropriate.
Results
Six hundred and fifty-nine new patient referrals were identified from nephrology clinic lists at Goulburn Valley Health within the defined three-year study period. Seventy-seven individuals were excluded from data collection: 48 were excluded because they failed to attend their new patient appointment and 29 were excluded for other reasons (Figure 1).
Of the 582 patients referred for specialist nephrology services who met the inclusion criteria, the mean age was 66.5 years (range: 16–99 years of age) and 281 were male (48.3%). Most patients (n = 527; 90.1%) were referred from primary care, whereas 41 (7.7%) were referred from other specialists and 13 (2.2%) were referred following an inpatient episode. Figure 2 details the distance patients travelled to attend the regional nephrology clinic.
 Figure 2. Distance travelled by patients to attend nephrology appointment and percentage of patients travelling these distances
Figure 2. Distance travelled by patients to attend nephrology appointment and percentage of patients travelling these distances
eGFR was included in 435 (74.7%) referrals and 298 (51.2%) noted sequential eGFR results. Renal imaging results were included in 201 (34.5%) referrals and blood pressure readings were noted in 100 (17.2%) referrals. Haemoglobin levels were detailed in 301 (51.7%) referrals and a parathyroid hormone level in 36 (5.9%) referrals. An ACR result was provided for 169 (29.0%) referrals and a further 54 (9.3%) referrals included a PCR result. Seventy (11.9%) referrals included urinalysis for red blood cells.
The data provided in referral letters described a clinical situation that met KHA-CARI guidelines for referral to nephrology services in 253 (43.5%) referrals. When data obtained at the initial nephrology clinic visit for eGFR and ACR/PCR were analysed, a further 82 referrals met KHA-CARI guidelines on the basis of these renal functional tests, bringing the total to 335 (57.6% of all referrals; Figure 3). The prevalence of comorbid cardiovascular disease and diabetes among the patient cohort is summarised in Table 1, along with medications of importance in the management of cardiovascular disease and hypertension among patients with CKD.
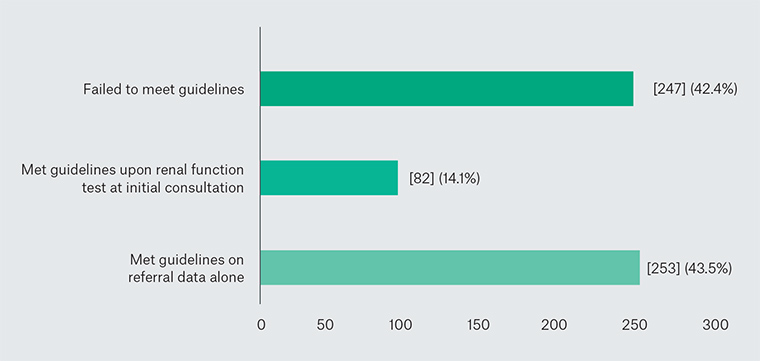 Figure 3. Referrals (number and percentage) meeting KHA-CARI guidelines on information available from referral letters, and eGFR and
Figure 3. Referrals (number and percentage) meeting KHA-CARI guidelines on information available from referral letters, and eGFR and
ACR/PCR at initial clinic visit
|
Table 1. Clinical data on comorbid conditions and medications delineated in referral letters
|
| Condition noted on referral* |
n (%) |
| Diabetes |
198 (34.0) |
| Unspecified cardiovascular disease |
183 (31.4) |
| Hypertension |
297 (51.0) |
| Ischaemic heart disease |
114 (19.6) |
| Congestive cardiac failure |
34 (5.9) |
| Peripheral vascular disease |
12 (2.1) |
| Abdominal aortic aneurysm |
5 (0.9) |
| Medications noted on referral† |
n (%) |
| Angiotensin converting enzyme inhibitors |
156 (26.8) |
| Angiotensin receptor blockers |
190 (32.6) |
| Diuretics |
140 (24.1) |
| Other antihypertensive agents |
249 (46.8) |
| Statins |
264 (45.4) |
*Multiple conditions may have been noted in referral letters
†Percentage refers to percentage of patients prescribed at least one of these medications |
Discussion
This study shows that 40% of referrals to a regional nephrology service did not meet CKD referral guidelines because of either insufficient information in the referral document or a clinical situation that did not meet referral guidelines. In some cases (n = 82), there was insufficient information in the referral document, but renal function tests performed at the initial consultation showed that patients did meet guidelines for referral. Some patients with inadequate referrals had declining renal function at the initial consultation. Valuable information, such as blood pressure and renal imaging, was absent from the majority of referrals.
These findings have a number of potential implications for this regional nephrology service. Firstly, if nephrologists only accepted referrals that met CKD referral guidelines, a substantial number of patients would not have received nephrologist appointments. Secondly, patients who did not meet referral guidelines may have been appropriately managed in the primary care setting. Thirdly, clinical judgement by the referring clinician and patient preference are important considerations, but these should be clearly articulated in the referral letter.
The results of this study are consistent with a study in a metropolitan nephrology service, which found that a quarter of referrals did not meet guidelines, and approximately a third of patients had their care transferred back to their referring primary care physician within six months.
18 Another study examined referrals during the 12 months after the introduction of eGFR reporting, and determined that only 65% of referrals were in line with referral guidelines.
17 A decade on from the incorporation of eGFR into reporting and referral guidelines, more than half of the referral letters examined in this study did not provide sufficient information to meet referral guidelines. Continuing education and training may be required to ensure key messages regarding CKD management and referral are kept current and consistent with peak body recommendations.
The nephrology workforce shortage in much of regional Australia makes it imperative that patients who would benefit most from specialist care are identified, and differentiated from patients who would be most appropriately managed in primary care. Service delivery for CKD nephrology services and its cost-effectiveness are under scrutiny.
19 A systematic review of available evidence
20 notes that there are still many gaps in the evidence for how to best manage patients with CKD, and further research is required.
Clearly, involving patients in referral decisions is likely to improve outpatient attendance, particularly for those travelling long distances to attend appointments, or for those who are frail. Previous work around the perspectives of patients, generalists and specialists towards referral and management options for patients with CKD
20 concluded that improving provision of referral information to specialists and emphasising the use of clinical guidelines were important improvements to CKD management.
This study demonstrates that in areas where secondary care services are in short supply, there is a need for primary and secondary care providers to collaborate to maximise efficient and effective service delivery. This shared approach ensures that crucial early investigations and interventions occur as part of CKD management, while timely referrals to nephrologists enable efficient provision of secondary nephrology services for the correct group of patients when they require it.
There may be a number of reasons why many nephrology referrals were not in line with CKD guidelines. Many Australian nephrology referral guidelines coexist, and although these guidelines are based largely on the same criteria, they may be confusing to referring clinicians. An online referral document to guide clinicians through the referral process and ensure essential investigations have been undertaken and reported may be warranted. This study found that an additional 14% of referrals met guidelines upon consideration of renal function results performed at initial consultation. This suggests that the clinical suspicion of the referring clinician was well placed, but communication via the referral letter was incomplete.
Implications for general practice
In this study, the majority of CKD referrals to a regional outpatient nephrology service contained insufficient detail to meet Australian guidelines; 40% of patients did not meet referral guidelines. The findings have implications on the provision of an efficient nephrology service in a region of nephrology workforce shortage, which must prioritise patients who are at greatest need and differentiate these patients from those who would be best managed in primary care. Inadequate referral information may result in some patients with CKD not receiving the recommended interventions, which may have the potential to prevent complications, and/or slow down progression of CKD in the future. It is now important that regional nephrologists, health services and primary care physicians work together to increase awareness of CKD referral guidelines, the rationale for them and the importance of their implementation.