Chest pain is a common complaint of patients presenting to primary care physicians and emergency departments. Given that some causes of chest pain are potentially lethal, the challenge is to make an accurate diagnosis.1 This article will focus on diagnosis and early management of patients with possible acute coronary syndrome (ACS). It will discuss key differentials that must be considered, and essential primary care investigations and management. Finally, hospital-based risk stratification and management will be described, providing an outline of what patients can expect from their referral to hospital.
Differential diagnosis of chest pain
A number of life-threatening and minor conditions may present with chest pain. Where minor conditions are confidently diagnosed, referral to the emergency department may not be necessary. Serious conditions include ACS, pulmonary embolism, aortic dissection and spontaneous pneumothorax (Box 1).2
| Box 1. Differential diagnosis of (non‑traumatic) chest pain* |
|
Life-threatening diagnoses
- Acute coronary syndrome (acute myocardial infarction, unstable angina pectoris)
- Pulmonary embolism
- Aortic dissection
- Spontaneous pneumothorax
Chronic conditions requiring urgent evaluation
- Angina pectoris due to stable coronary artery disease
- Aortic stenosis
- Aortic aneurysm
- Lung cancer
Other acute conditions
- Acute pericarditis
- Pneumonia or pleurisy
- Herpes zoster
- Peptic ulcer disease
- Gastro-oesophageal reflux
- Acute cholecystitis
Other diagnoses
- Neuromusculoskeletal causes
- Psychological causes
|
*This differential diagnosis is not intended to be exhaustive
Adapted with permission from the Medical Journal of Australia, from Parsonage WA, Cullen L and Younger JF. The approach to patients with possible cardiac chest pain. Med J Aust 2013;199(1):30–34. |
Pulmonary embolism (PE) risk factors include the presence or clinical suspicion of deep vein thrombosis (DVT), past history of DVT/PE, active malignancy, recent trauma, surgery or immobility, and use of exogenous oestrogen. Generally, patients complain of a sharp pleuritic pain, and may be short of breath or have haemoptysis, tachycardia and hypoxemia. The electrocardiogram (ECG) may be normal or show non-specific changes including, tachycardia, S1Q3T3 (S wave in lead I, Q wave and T wave inversion in lead III), incomplete/complete right bundle branch block, right axis deviation, inverted T-wave (V2–3), peaked P waves and atrial flutter. Decision rules such as the Wells score or pulmonary embolism rule-out criteria (PERC) assist in determining the probability of pulmonary embolus and guide the use of D-dimer testing and clinical management. A negative D-dimer using quantitative enzyme-linked immunoabsorbent assay (ELISA) effectively excludes PE in patients with low pretest probability.3 Definitive diagnosis is made with computed tomography pulmonary angiography (CTPA) in most cases.
Risk factors for aortic dissection include smoking and cocaine use, connective tissue disorders, infection and inflammation, atherosclerosis, previous heart or aortic valve surgery, bicuspid aortic valves, blunt trauma and pregnancy. The pain is typically sudden-onset and described as a tearing or ripping pain radiating through to the inter-scapular area and associated with dyspnoea, syncope, neurological symptoms or abdominal pain. Physical examination may be entirely normal or reveal hypertension, neurological deficits, peripheral ischaemia, blood pressure or pulse differentials between right and left sides, and new murmurs/muffled heart sounds/pericardial friction rub/jugular venous distension. On suspicion of this diagnosis, the patient should be treated as a medical emergency with immediate referral and transport to hospital by an appropriate prehospital provider. The definitive diagnosis is made using CT aortography.
Spontaneous pneumothorax may occur with underlying lung disease or trauma (secondary), or without (primary), and patients will present with sudden chest pain and/or shortness of breath. Respiratory distress may be minor or significant. On examination, a resonant percussion note and decreased breath sounds may be found. Radiological investigation will provide the diagnosis. Tension pneumothorax can rarely occur in spontaneous pneumothorax and is a surgical emergency. Any suggestion of haemodynamic instability or mediastinal shift requires immediate decompression.
Of the most common life-threatening causes of chest pain, ACS cannot be diagnosed on history or clinical examination alone.4 Many patients do not present with the classic symptom of severe or crushing central chest pain exacerbated by exertion and that radiates to the arms, neck or jaw, and is associated with sweating, nausea and shortness of breath.4 Elderly patients, women and patients with diabetes more frequently present with atypical symptoms.5 The presence or absence of risk factors for ACS (family history of ischaemic heart disease, smoking, hypertension, hyperlipidemia) does not help rule in or rule out ACS for individual patients. Similarly, physical examination is frequently normal and cannot be relied upon for diagnosis.4–6
The assessment and management of patients with suspected ACS in the primary care setting should include determining the urgency of need for referral. If patients have had any ongoing symptoms within the preceding 24 hours, they should be referred immediately to an emergency department for assessment.7
Primary care investigations for suspected ACS
The ECG
An ECG should be performed within 10 minutes of assessing a patient with suspected ACS for identification of ST-elevation myocardial infarction (STEMI). Such patients require immediate referral via ambulance services to hospital to enable urgent reperfusion therapies to be commenced.2,5 It is recommended that all general practices have a system in place to ensure rapid clinical review of ECGs.
Typical ECG findings in STEMI include ST segment elevation and reciprocal ST segment depression in other leads. An exception to this is the posterior infarction where ST depression in leads V1 to V3 is the predominant abnormality (Figure 1). Another ECG variation occurs with proximal coronary artery occlusion, where the ECG may show widespread ST depression with elevation only in leads aVR and V1. In right ventricular infarction, ST segment elevation is seen in V1, V2 and V3 (Figure 2). This is a significant pattern to recognise as the administration of glyceryl trinitrate (GTN) can reduce preload enough to cause serious haemodynamic compromise.4,7,8 The ECG may show other patterns suggestive of ischaemia, including ST segment depression, T wave flattening or inversion, or hyperacute T waves (peaked) (Figure 3).8,9 Online resources may contribute to clinicians’ knowledge.10
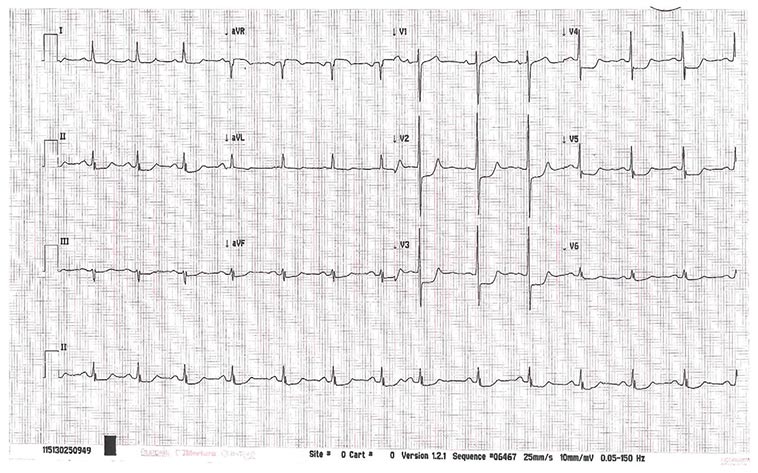
Figure 1. ECG showing posterior myocardial infarction
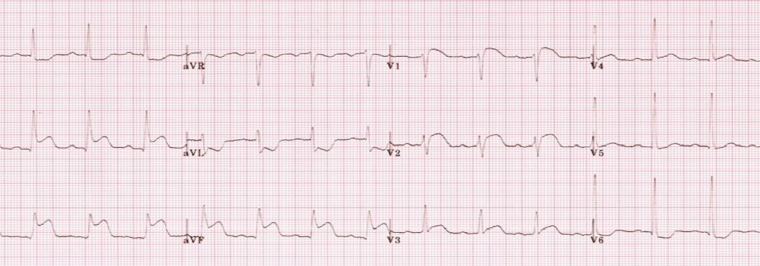 Figure 2. ECG showing inferior and right ventricular myocardial infarction with ST elevation
Figure 2. ECG showing inferior and right ventricular myocardial infarction with ST elevation
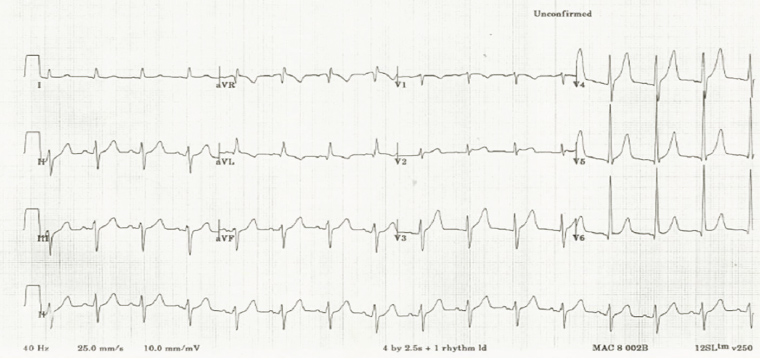
Figure 3. ECG showing hyperacute T waves
Troponin
Troponin is a structural protein unique to cardiac myocytes, detected following acute myocardial infarction (AMI). The presence of troponin indicates cardiac muscle injury or necrosis. In patients with suspected ACS, single troponin testing in the primary care setting is rarely indicated. Patients with any symptoms within the preceding 24 hours should be referred immediately to an emergency department for assessment.7 Patients who have been symptom-free for between 24 hours and 14 days previously and who have no high-risk features (ongoing or recurrent pain, syncope, heart failure, abnormal ECG) may be investigated using troponin testing;7 however, general practitioner–initiated troponin testing has been shown to place patients at high risk of adverse outcomes, even when the cardiac troponin test result is negative.11 For this reason, caution is recommended in the use of troponin testing in the non-rural primary care setting.
Primary care physicians in a rural or remote setting may have requirements for troponin testing, which is usually performed with point-of-care assays. This result will support physicians in determining the degree of urgency with which a patient should be referred or transferred to definitive care.
Referral and ongoing management in primary care
Patients with suspected ACS, including new-onset angina, should be referred urgently to the nearest emergency department. Patients identified as having a STEMI or ongoing chest pain, dyspnoea, syncope/presyncope or palpitations should be transferred as an emergency via ambulance.5 Many ambulance services have capability to directly transmit 12-lead ECGs to the hospital (emergency department and interventional cardiologist), enabling direct transfer of patients to the cardiology catheter laboratory. Therefore, expediting contact with ambulance services is critical to support reduction in door-to-device time.12 In all other scenarios, patients should be advised not to drive themselves. While awaiting transfer, management should occur, provided transport to hospital is not delayed. Referral to an emergency department is best done by direct phone call to the hospital while ambulance transport is arranged for the patient. Supporting documentation should include the patient’s ECG recordings.
Some aspects of the initial management of patients with proven or suspected ACS have been recently updated.5 Routine use of oxygen is no longer recommended unless oxygen saturations are measured at <93% (<88–92% in chronic obstructive airways disease [COAD] to maintain hypoxic drive).5,13 GTN should be administered to symptomatic patients whose chest pain is thought to be caused by ACS. The exceptions to this include cases with suspected right ventricular myocardial infarction, or if the patient has recently taken a phosphodiesterase type 5 inhibitor (eg sildenafil, tadalafil), as the combined effect can cause precipitous and severe hypotension.5 The dose is 0.3–0.6 mg (tablet) or 0.4–0.8 mg (spray) sublingually every five minutes for three doses. Oral aspirin, 300 mg, should be given to all with suspected ACS as it significantly decreases the risk of serious vascular events, including myocardial infarction and stroke, without observable increases in the risk of bleeding. The only absolute contraindication is hypersensitivity.5
Intravenous opioids are recommended to treat pain that does not respond to GTN, but recent research suggests that morphine may decrease the absorption of oral anti-platelet agents.5,14 For this reason, fentanyl is the preferred opioid for analgesia in suspected ACS.
Hospital-based risk stratification for ACS
Further assessment, including risk stratification for ACS, will occur in hospital. The National Heart Foundation and Cardiac Society of Australia and New Zealand 2016 risk classification for suspected cardiac causes of chest pain classifies patients as high, intermediate or low risk.5 The classification includes features of history and examination, as well as investigations such as troponin and ECG results (Box 2). There are other risk stratification scoring systems in use worldwide; the most common include TIMI,15,16 GRACE17 and HEART18 scores. However, none of these have been assessed for use in the primary care setting.
| Box 2. National Heart Foundation and Cardiac Society of Australia and New Zealand risk classification for possible cardiac causes of chest pain |
|
High risk
- Ongoing or recurrent chest discomfort despite initial treatment
- Elevated cardiac troponin level
- New ischaemic changes on electrocardiogram (ECG), such as persistent or dynamic ECG changes of ST segment depression ≥0.5 mm; transient ST segment elevation (≥0.5 mm) or new T wave inversion ≥2 mm in more than two contiguous leads; or ECG criteria consistent with Wellens syndrome
- Diaphoresis
- Haemodynamic compromise — systolic blood pressure <90 mmHg, cool peripheries, Killip Class >I and/or new-onset mitral regurgitation
- Sustained ventricular tachycardia
- Syncope
- Known left ventricular systolic dysfunction (left ventricular ejection fraction <40%)
- Prior acute myocardial infarction, percutaneous coronary intervention or coronary artery bypass grafting
Low risk
- Age <40 years
- Symptoms atypical for angina
- Remain symptom free
- Absence of known coronary artery disease
- Normal troponin level
- Normal ECG
Intermediate risk
|
| Adapted with permission from Elsevier, from Chew DP, Scott IA, Cullen L, et al. National Heart Foundation of Australia & Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of acute coronary syndromes 2016. Heart Lung Circ 2016;25(9):895–951. |
As a single troponin test is not able to rule out AMI in patients presenting acutely with suspected ACS, serial testing is performed. A delay of up to three hours for troponin release to be detected in the setting of AMI may occur.5 The finding of an elevated troponin value also does not rule in AMI, with many causes of elevated troponin identified (Box 3).7 This demonstrates the need for a contextual approach to troponin testing, as well as for serial sampling (to evaluate if a rise and fall pattern in troponin values occurs over time).19 Serial ECGs are also performed, and some patients may require ongoing ECG monitoring during their assessment and management.
| Box 3. Causes of elevated serum troponin level |
Cardiac
- Acute myocardial infarction
- Coronary artery spasm (eg due to cocaine or methamphetamine use)
- Takotsubo cardiomyopathy
- Coronary vasculitis (eg systemic lupus erythematosus, Kawasaki disease)
- Acute or chronic heart failure
- Tachyarrhythmia or bradyarrhythmia
- Frequent defibrillator shocks
- Cardiac contusion or surgery
- Rhabdomyolysis with cardiac involvement
- Myocarditis or infiltrative diseases (eg amyloidosis, sarcoidosis, haemochromatosis)
- Cardiac allograft rejection
- Hypertrophic cardiomyopathy
Non-cardiac
- Cardiotoxic agents (eg anthracyclines, trastuzumab, carbon monoxide poisoning)
- Aortic dissection or severe aortic valve disease
- Severe hypotension or hypertension (eg haemorrhagic shock, hypertensive emergency)
- Severe pulmonary embolism, pulmonary hypertension or respiratory failure
- Dialysis-dependent renal failure
- Severe burns affecting >30% of the body surface
- Severe acute neurological conditions (eg stroke, cerebral bleeding or trauma)
- Sepsis
- Prolonged exercise or extreme exertion (eg marathon running)
|
| Adapted from Aroney CN and Cullen C. Appropriate use of serum troponin testing in general practice: A narrative review. Med J Aust 2016;205(2):91–94. © Copyright 2016 The Medical Journal of Australia – reproduced with permission. |
Individual health services should use a protocol for the risk stratification and subsequent assessment of patients with suspected ACS, which may include exercise stress testing, myocardial perfusion scanning, stress echocardiography or computed tomographic coronary angiography. Further management in the case of proven ACS that may be instituted in hospital include medical therapies, interventional cardiology procedures such as percutaneous coronary intervention (PCI) and surgical options (eg coronary artery bypass graft [CABG]). In patients with STEMI angiography with coronary revascularisation, PCI or CABG is the treatment of choice, or fibrinolysis (if PCI is unavailable within 90 minutes) followed by angiography +/– PCI within 24 hours.5
Conclusion
ACS is common and life-threatening, and must be considered in all patients with chest pain who present to general practice. A focused history and examination will define high-risk patients; however, this will not exclude a diagnosis of ACS. An ECG is the key immediate investigation primary care physicians must obtain. Close liaison with the nearest emergency department will ensure further risk stratification and that optimum management can be started as early as possible.