Case
A mother presented with her four-year-old daughter with persistent concerns of ongoing abdominal pain. It was difficult for the daughter to describe the pain, but her mother stated it could bring her to tears. She had been having the pain on a daily basis for several months and it could occur at any time with no clear trigger. On direct questioning, her mother believed her daughter passed a motion daily and reported no diarrhoea, denied constipation and stated there was no blood or mucus in the stool. There were no urinary symptoms and the girl was otherwise well, born at term and meeting her developmental milestones with no other significant medical history.
Given the chronic, recurrent and severe nature of the pain, an ultrasound was organised. An extract from the report read:
Incidentally, there is reversal of the orientation of the superior mesenteric artery and superior mesenteric vein, which can be viewed in the context of malrotation. Paediatric opinion is advised.
Question 1
What is the cause of malrotation?
Question 2
How frequently do malrotations occur? Is there an association with other abnormalities?
Question 3
At what age and with what symptoms do symptomatic malrotations present?
Question 4
What imaging is most appropriate for diagnosis?
Question 5
What is the treatment for this condition?
Answer 1
Malrotation occurs when there is an error in the embryonic midgut development, which takes place during weeks 4–10 of gestation.1,2 During this sequence of complex events, the developing bowel protrudes from the abdominal cavity and rotates as it returns.1 Malrotation occurs if there is an error with this process and the caecum comes to rest in a position other than the right lower quadrant (typically, the right upper quadrant or mid-epigastrium).1 However, it is not the abnormal location alone that predisposes to complications; it is also that the bowel is not normally fixated.1
Answer 2
Malrotation is the most frequent developmental abnormality of the small intestine.3 It is estimated that one in 200 live births have an abnormality of this development, but only one in 6000 live births have symptomatic malrotation.3
Malrotation may occur alone or in association with another congenital abnormality.4 Other conditions where the embryological midgut does return to the abdomen, such as gastroschisis, diaphragmatic hernias and omphalocele, generally have an associated malrotation.4 In addition, children who have heterotaxy, a condition of varying severity where the internal organ/s are not in their usual left and right positions, are at increased risk of malrotation.4
Answer 3
Initial presentation of symptomatic malrotation can be in childhood or adulthood. However, 80% of symptomatic cases will present with bilious vomiting within the first few weeks of life.1 Presentations beyond the neonatal period tend to manifest with more varied and less specific symptoms, including gastroesophageal reflux disorder (GORD), acute or chronic abdominal pain, diarrhoea, constipation, non-bilious vomiting or haematochezia.1
Answer 4
In an acutely unwell child, abdominal X-ray is an appropriate initial imaging modality, aimed at identifying any suspected bowel obstruction.3 In a child who is not acutely unwell, ultrasonography is an appropriate initial screening mechanism, and an experienced sonographer is able to identify the reversed position of the superior mesenteric artery and vein (Figure 1).5 Confirming malrotation can be difficult, and further evaluation with an upper gastrointestinal series after specialist review is generally required.1 This investigation must be examined carefully by an appropriate specialist, as there is significant potential to confuse normal anatomical variation for malrotation.1
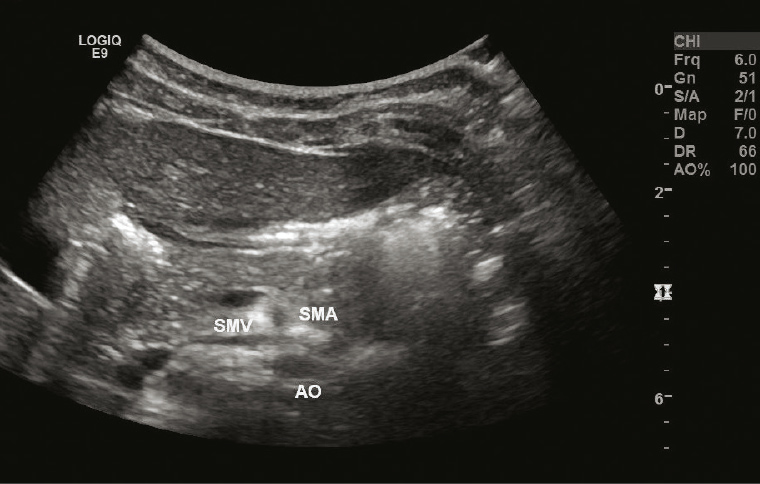
Figure 1. Abdominal ultrasound showing the reverse positioning of the superior mesenteric artery and vein
Answer 5
If volvulus is present, surgical correction is mandated.2 However, given the potential for significant and possibly life-threatening complications of malrotation, surgical correction is considered for confirmed malrotation even if there has been no acute presentation.2 For this reason, specialist opinion is essential.
Surgical correction involves a laparoscopic approach known as Ladd’s procedure.2 An appendectomy is generally performed during this procedure as the appendix will otherwise be abnormally positioned.2
Key points
- Malrotation is common, but the vast majority of malrotations are asymptomatic.
- Symptomatic malrotation can present at any age, but 80% of symptomatic cases present in the first few weeks of life with bilious vomiting.
- The potential for the life-threatening complication of volvulus mandates specialist review for further evaluation when malrotation is identified.