Discussion
In the absence of organic aetiology, childhood constipation is almost always functional and often due to painful bowel movements that prompt the child to withhold stool. It is important to initiate a clear management plan for the family, as what is an easily treatable condition can escalate into a vicious cycle of pain if not addressed early. The medical approach should consider organic disease, the use of appropriate toileting habits, and dietary modifications. Laxatives are often required to re-establish regular, painless defaecation.
This article is the second in a series on paediatric health. Articles in this series aim to provide information about diagnosis and management of presentations in infants, toddlers and pre-school children in general practice.
Within the first three months of life, infants can pass anywhere from 5 to 40 motions per week, decreasing at age one year to 4–20 motions per week and at three years to 3–14 per week.1–4 The Rome IV criteria are applied in order to formally define functional constipation. Constipation under these criteria requires two or more of the following:3
- two or fewer defaecations per week
- at least one episode of faecal incontinence per week
- history of retentive posturing or excessive volitional stool retention
- history of painful or hard bowel movements
- presence of a large faecal mass in the rectum
- history of large diameter stools that may obstruct the toilet
- symptoms occurring at least once per month for a minimum of one month, with insufficient criteria to diagnose irritable bowel syndrome.
Faecal incontinence refers to the passage of stools in an inappropriate place, and may result from chronic retention of stool with passive overflow during withholding.3 Parents can interpret this passage of stool as the child trying to defaecate; it is more likely that this incontinence is due to strong colonic contractions attempting to expel stool while the child is withholding, especially if there is associated retentive posturing.3 The presence of abdominal pain, distension, behaviour change and anorexia in these children may indicate a need for disimpaction.3 Organic causes of incontinence include spinal cord or sphincter anomalies (Box 1).3
|
Box 1. Organic causes of constipation3
|
| Allergy – cow’s milk protein intolerance and/or other food protein intolerances |
| Coeliac disease |
| Hypothyroidism |
| Cystic fibrosis |
| Electrolyte abnormalities – hypercalcaemia, hyperkalaemia |
| Drugs – opiates, phenobarbital, anticholinergics |
| Neuropathic disorders – Hirschsprung’s disease, internal sphincter achalasia |
Spinal cord abnormalities – myelomeningocele, tethered spinal cord, syringomyelia
Stooling may occur without sensation or urge |
| Anatomic malformations – imperforate anus, anteriorly displaced anus |
Key points in the history
- When was the onset of constipation or soiling? What was the duration?
- What is the form and calibre of motions, frequency and relation to daily activity?
- Is there suspicion of an organic cause, or red flags in the history (Box 1, Box 2)?
- Has the child been toilet-trained for stooling and/or urination?
- When and how often does the child sit on the toilet?
- What is the toileting posture? Are both feet resting on the ground or footstool and the child leaning forward with a relaxed abdomen?
- Are there triggering events (eg disrupted routine, entering day care or an episode of painful, hard stools leading to withholding)?
- Are there any neurodevelopmental concerns? Children with developmental delay or behavioural disorders will require additional help to be toilet trained.
| Box 2. Red flags in the history3 |
| Blood in stools |
| Systemic symptoms – faltering growth, weight loss, lethargy |
| Perianal disease |
| Extra-intestinal symptoms suspicious for inflammatory bowel disease – rashes; arthritis; red, sore eyes; mouth ulcers |
| Delayed passage of meconium after the first 48 hours of life, infrequent stools with straining and/or thin, strip-like stools (suspicious of Hirschsprung’s disease) |
| Urinary symptoms |
| Abnormal lower limb neurology |
| Patulous anus |
| Absent perineal sensation |
| Onset of constipation before one month of age |
Determine the presence of any withholding behaviours. These include:
- going stiff
- clenching buttocks
- walking on tip toes
- crossing legs
- bracing against furniture
- being in all fours position or curling up in a ball
- sitting with legs straight out.
Could this be allergy?
Constipation can be associated with food allergy, particularly to cow’s milk. A dietary history is essential and should include the mother if the child is still being breastfed. Cow’s milk protein can be found in breast milk, formula and dairy-containing solids. Factors that may indicate a cow’s milk protein intolerance are outlined in Box 3.5–7 For infants aged <1 year, the evidence-based Cow’s milk–related Symptom Score (CoMISS) can be helpful.8,9 This can be calculated on a smartphone app called GIdiApp (gastrointestinal diseases app), which covers assessment and management of functional gastrointestinal symptoms in babies.8,9 A three-day diary of diet and stooling patterns can be useful for parents and general practitioners.
| Box 3. Factors associated with cow’s milk protein intolerance5–7 |
| Onset of symptoms on changing from breast to bottle feeds |
| Onset of symptoms on starting cow’s milk |
| Onset of symptoms on starting solid foods |
| Medication-resistant or medication-dependent constipation |
| Straining during defaecation, even in the presence of soft stools |
| Atopic disease – eczema, asthma, rhinitis |
| Rashes/urticarial with milk feeds/food |
| Irritability in infancy – reflux or vomiting |
| Voluntary dairy restriction |
| Family history – atopy, food allergy, food intolerance, autoimmune conditions |
Physical examination
Examination should focus on the following:1
- identify ‘red flags’
- abdominal exam – assess for faecal masses
- inspect the anus – look for patency, fissures, patulous anus, anteriorly placed anus
- neurological exam – assess the back, gait, lower limb tone, power, reflexes and plantar responses. Note that guidelines do not support the use of a digital rectal examination to diagnose functional constipation.3,4
Investigations
Assessment for coeliac disease, hypothyroidism and hypercalcaemia is not recommended in children without alarm symptoms. Testing, if required, includes immunoglobulin A (IgA), tissue transglutaminase (tTG) IgA, thyroid function, calcium and electrolytes.1–3 Coeliac disease may be considered if constipation arises early on with the introduction of gluten, and is associated with iron deficiency anaemia, abdominal pain and poor growth.3 Abdominal X-ray is not recommended to diagnose functional constipation, and magnetic resonance imaging of the spine is not required in those without neurological abnormalities in the primary care setting.3
In infants aged <1 month, faecal impaction is rare and may be related to an underlying cause such as Hirschsprung’s disease.3 Exclusively breastfed babies defaecate anywhere from five times per day to once a week, and a decrease in stooling may be normal or abnormal.4 Referral for rectal biopsy to a tertiary paediatric facility should be considered if there is a clear history of not passing meconium with the first 48 hours of life or of ongoing thin, strip-like stools.3
Diet
Allergy testing is not recommended to diagnose suspected cow’s milk allergy in children with constipation, as it is usually not IgE mediated.10 A one-month trial of avoidng cow’s milk and soy protein may be indicated in children with intractable constipation.3 During this period, calcium intake should be supplemented with almond or rice products, or calcium supplementation.11 Dairy intolerance can improve with time in older children but data in small children is limited.10 Dairy is tried in the diet every 6–12 months as tolerated. Referral should be made to a paediatrician or paediatric gastroenterologist/allergist if there is suspicion of multi-food allergies. Normal fibre intake, fluid intake and exercise are recommended for children with constipation. Fibre supplements are not recommended.3
Management of functional constipation
For children who are not yet toilet-trained for stool, and who feel more secure defaecating in a diaper, this should be encouraged while the stool is softened with laxatives and the child regains confidence. Toilet training should be child‑led. Routine is important; if old enough to comply, children should be encouraged to sit on the toilet for five minutes after every meal. This can be used in conjunction with a rewards program such as a star chart.
Drug therapy
Goals of drug therapy are to soften stools to eliminate the child’s fear of painful defaecation. When discussing medication with parents, it is important they understand that the bowel does not become ‘dependent’ on the medication.1,2 Insufficient treatment can lead to long-term bowel damage from impacted stool. Also, parents need to know that the stool will be made artificially soft, almost like diarrhoea, to allow the ‘stretched pipes’ to return to normal size, shape and function.
Reasons for treatment failure should be explained. These include insufficient dose and duration, poor compliance, recurrence of trigger factors or alternative diagnosis. Compliance may be affected by the taste and amount of laxative the child is required to drink. Oral polyethylene glycol (PEG) 3350 with or without electrolytes (Movicol, Clearlax or Osmolax; Table 1) is the most effective first-line treatment for disimpaction in the outpatient setting.
1,3,4 PEG has also been shown to be effective in infants aged <1 year, but evidence is limited.
1,12 One sachet of Movicol contains 13.1 g of PEG, one sachet of Movicol Junior contains 6.5 g, and one scoop of Osmolax contains 8.5 g. Movicol also contains sodium chloride (350 mg), sodium bicarbonate (178 mg) and potassium chloride (50 mg) per sachet and comes in lemon-lime and chocolate flavours. Osmolax doesn’t contain electrolytes and is often preferred due to its tasteless nature. PEG with electrolytes is often used when required in large volumes via nasogastric tube in hospital.
3 Rectal therapies, such as enemas, are rarely required and do not accelerate recovery.
| Table 1. Laxatives and doses3,13 |
| Laxative |
Dosage |
Side effects |
| Osmotic oral |
|
|
| Polyethylene glycol (PEG) 3350 |
Disimpaction: 1–1.5 g/kg/day for three days Maintenance: 0.75 g/kg/day |
Abdominal cramps and nausea |
| Lactulose |
1–3 mL/kg/day in divided doses
(3.3 g/5 mL) |
Flatulence, abdominal cramps; less effective than PEG or paraffin oil |
| Liquid paraffin 50% (Parachoc) |
12 months–6 years: 10–15 mL/day
7–12 years: 20 mL daily |
Pneumonia if aspirated (children with reflux or unsafe swallow are at risk) |
| Stimulants |
|
|
| Senna |
2–6 years: 2.5–7.5 mL/day
6–12 years: 5–15 mL/day
Syrup – 7.5 g/5 mL
Tablet – 1 tablet = 7.5 mg |
|
| Bisacodyl |
4–18 years: 5–20 mg/day oral
2–18 years: 5–10 mg rectally once per day |
|
| Picosulfate |
1 month – 4 years: 2.5–10 mg/day
4–18 years: 2.5–20 mg once per day |
|
Disimpaction
Treatment of constipation is not effective if faecal impaction is not treated. Disimpaction dose for children is 1–1.5 g/kg/day of PEG for 3–6 days.1,4 Maintenance therapy is 0.75 g/kg/day.10,13,14 If PEG is not available or tolerated, the next most appropriate laxative is liquid paraffin, available commercially under a number of brands (eg Parachoc).3 Schools should be made aware of the new therapy and medication started over the weekend or school holidays. Children should be allowed immediate access to the toilet if they feel the call to stool.
Maintenance
In the case of chronic constipation, families should continue with PEG and aim for extra soft stools, type 5 or 6 on the Bristol stool scale.1 Poor sensation and motor function from chronic constipation may mean it will take months of emptying soft stool to regain normal function.1–3 Once a child is defaecating without discomfort, families can titrate the medication to achieve ideal stool softness.1 It is useful for the family to understand that PEG softens the stool by drawing in fluid via osmosis and passes through the bowel without being absorbed into the body.14
Children will often need three months of treatment if they have had a previously normal bowel habit, a short duration of symptoms (less than three months) and are toilet trained. Children with a chronic history will often need at least six months of treatment.3 Withholding behaviours, an ongoing trigger event and the absence of toilet training can lead to longer treatment.3 Constipation should be resolved for at least one month before treatment is ceased.3
Stimulants
If a brief period of constipation occurs while on adequate softener treatment, a stimulant laxative can be added. Stimulants can also be trialled if adequate disimpaction is not achieved after two weeks on PEG.1
When to refer to allied health
If needing additional help with toileting, children with a developmental age >4 years may benefit from referral to an occupational therapist or continence physiotherapist. The Continence Foundation of Australia
(www.continence.org.au) provides support for families with constipated children.
When to refer to the paediatrician
Consider if constipation is medication-dependent after six months of adequate treatment, or if medication resistant or organic causes have been considered (Figure 1).3 Further management may include allergy diets, specialist pelvic floor training, colonic transit studies, anal manometry and rectal biopsy.3
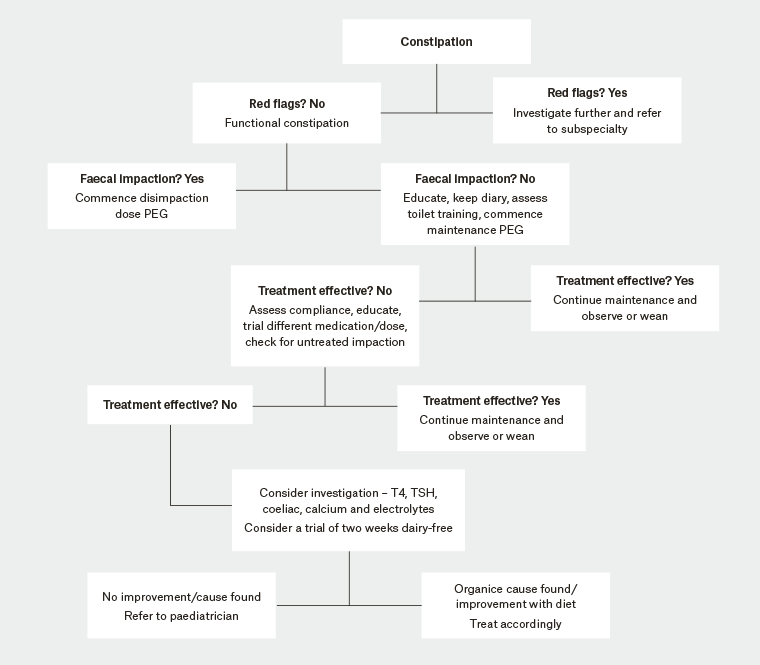 Figure 1. Management of constipation3,15
Figure 1. Management of constipation3,15
PEG, polyethylene glycol; T4, thyroxine; TSH, thyroid-stimulating hormone
Prognosis and conclusion
Up to 50% of patients referred to a paediatrician for constipation will regain normal function and be off laxatives in six to 12 months.3 Eighty per cent of children treated early in their course will recover without use of laxatives at six-month follow-up, in comparison with 32% of children with a delay in their treatment.3 Early therapeutic intervention is beneficial and easy to commence. Close follow-up is important for good results.