The opinions expressed by correspondents in this column are not endorsed by the editors or The Royal Australian College of General Practitioners.
Global climate change and the public health consequences
Congratulations to Dr Parise and Australian Journal of General Practice for publishing a comprehensive summary of climate change science, the public health impact, inequity of risk and how we should respond (AJGP July 2018).1 Many of the strategies that Dr Parise has identified, such as urban planning, public health infrastructure and improved local ecosystem management, are outside the scope of day-to-day general practice. However, to complement these strategies, general practitioners (GPs) can act both personally and professionally. Our roles as community leaders and trusted experts increase the importance of our actions and make it easier for others to respond. Many responses to climate change have wide-ranging benefits.
Active transport, through walking, cycling and using public transport, reduces both carbon and particulate pollution, traffic congestion and motor vehicle crashes, and increases physical activity and the amenity of our streets. Consuming locally grown fruit and vegetables builds skills, increases demand for such produce, reduces food transport, waste and processing, and improves diets and knowledge of food production.2 Low-carbon holidays and using telecommunications rather than air travel significantly reduce carbon emissions.3 Asking about pregnancy intentions and providing contraceptive advice to women supports rights to reproductive control, provides opportunity for pre-pregnancy care and prevents unwanted pregnancy: the impact on climate change is a co-benefit.3,4
Acting together and advocating for changes in policy, industry and investment are needed for regional, national and global responses to climate change. Besides the professional and community organisations that Dr Parise mentions, GPs could work with Doctors for the Environment Australia (DEA).5 Climate change, the greatest threat to public health, is a focus of DEA activities.
Dr Rosalie Schultz MPH,
FAFPHM, FRACGP, FARGP
PhD Student, Centre for Remote Health, Flinders University, SA
Declaration: RS is supported by a Vincent Fairfax Family Foundation Scholarship and a spokesperson for the DEA.
References
- Parise I. A brief review of global climate change and the public health consequences. Aust J Gen Pract 2018;47(7):451–56. doi: 10.31128/AJGP-11-17-4412.
- Lowe M. Obesity and climate change mitigation in Australia: Overview and analysis of policies with co-benefits. Aust N Z J Public Health 2014;38(1):19–24. doi: 10.1111/1753-6405.12150.
- Wynes S, Nicholas K. The climate mitigation gap: Education and government recommendations miss the most effective individual actions. Env Res Lett 2017;12:074024. doi: 10.1088/1748-9326/aa7541.
- Bellanca HK, Hunter MS. ONE KEY QUESTION®: Preventive reproductive health is part of high quality primary care. Contraception 2013;88(1):3–6. doi: 10.1016/j.contraception.2013.05.003.
- Doctors for the Environment Australia. About DEA: About us. College Park, SA: DEA, 2018. Available at www.dea.org.au/about-dea [Accessed 1 August 2018].
Stigmatising language
I would like to register my concern at the stigmatising language used in the article, ‘Developing a general practice workforce for the future’ by Hays and Gupta (AJGP August 2018).1 In this article, the authors use the term ‘drug addicts’. This term is stigmatising and dehumanising, and I am disappointed to find it in a peer-reviewed article. I draw your attention to a pamphlet, Language Matters,2 which suggests instead: ‘people with a dependence on drugs and alcohol’. This pamphlet was developed by people with lived experience of dependence on drugs and alcohol. It draws on work previously carried out in New Zealand3 and the United States,4 and it is part of the process of working towards decreasing stigma. This stigma is perpetuated by the language we use and is one of the reasons that people with a dependence on drugs and alcohol are underserved, as suggested in the article by Hays and Gupta.1
Dr Hester Wilson
The Langton Centre
Surry Hills, NSW
References
- Hays R, Gupta TS. Developing a general practice workforce for the future. Aust J Gen Pract 2018;47(8):502–05.
- Network of Alcohol and other Drugs Agencies, NSW Users and Aids Association (NUAA). Language matters. NSW: NADA and NUAA, 2017. Available at www.nada.org.au/resources/language-matters [Accessed 18 September 2018].
- Matua Raki. Language matters (poster). Wellington: Matua Raki, 2016. Available at www.matuaraki.org.nz/resources/Language%20matters%20poster/696 [Accessed 18 September 2018].
- National Council for Behavioural Health. Language matters. Washington DC: National Council for Behavioural Health, 2015. Available at www.thenationalcouncil.org/surgeon-general-toolkit/language-matters [Accessed 18 September 2018].
Editorial note: The online version of this article has been adjusted accordingly.
A simple technique for controlling the non-viewing eye during direct ophthalmoscopy
Ophthalmoscopy is used to examine the ocular fundus. It may reveal important changes in patients with diabetes mellitus, hypertension and headache. The direct ophthalmoscopic examination is, therefore, often integral to the physical examination.
The examination is undertaken in a dimly lit room and the patient is instructed to focus on a distant object. The direct ophthalmoscope is held in the right hand and the right eye used to examine the patient’s right eye, while closing the left eye. This sequence is reversed to examine the patient’s left eye.1 For right-handed examiners, who are generally right-eye dominant, closing or suppressing the right eye while examining the patient’s left eye can be difficult. Many ophthalmologists will develop ways to overcome this. We propose an alternative technique that is effective and relatively easy to achieve. To our knowledge this method has not been described previously.
Suggested technique
This simple technique allows for direct ophthalmoscopy without having to close or suppress the non-viewing eye.
We find this technique useful for teaching ophthalmoscopy, as dominant eye closure or suppression problems are common among students. Those who may not be using ophthalmoscopy frequently, such as general practitioners or physicians, may also find this technique helpful.
Ying Jo Khoo
MBBS,University of Western Australia, WA
Andrea Meehan
MBBS, BMedSci (Hons), RACP,
University of Western Australia,
Perth Children’s Hospital for Children, WA
Philip House
MBBS, FRANZCO, AM, University of Western Australia, Applecross Eye Clinic, WA
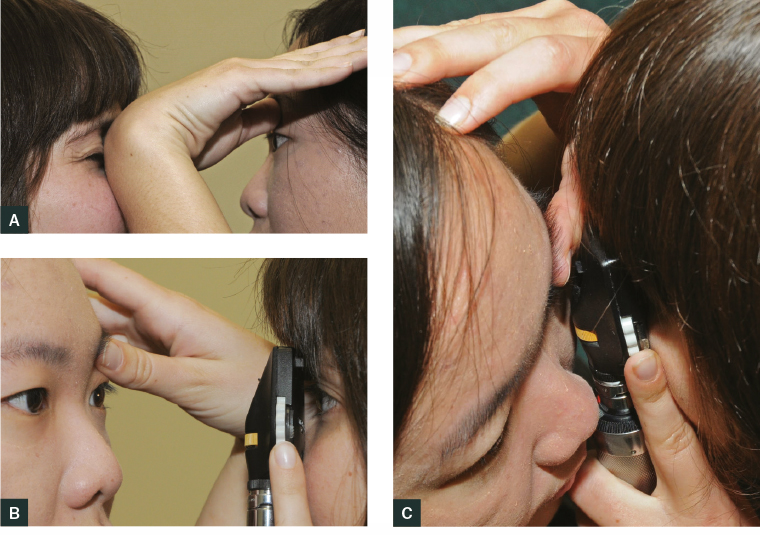
Figure 1. Technique for teaching ophthalmoscopy
A. To examine the left eye, with the right thumb anchored on the patient’s left brow, the dorsal aspect of the right wrist is brought towards the examiner’s non-viewing (right) eye to block the vision.
B. As the examiner moves closer to the patient, the wrist occluding the non-viewing eye relaxes to allow the viewer to closely approach the subject.
C. The ophthalmoscope should touch the examiner’s thumb, which is holding the upper lid. This proximity will optimise visualisation of the retina. The technique is reversed for the right eye.
Acknowledgement
We would like to express our appreciation to Mr Chris Barry, ophthalmic photographer, for his assistance with the photographs.
References
- James B, Benjamin L. Examination of the retina and optic disc. In: Ophthalmology: Investigation and examination techniques. Philadelphia: Elsevier, 2007; p. 45–57.