Palpitations are one of the most common presentations to general practice, and while they are usually benign, they may also have life-threatening significance. Palpitations have been estimated to account for 16% of general practice presentations and are the second most common presentation to cardiologists after chest pain.1 Although the vast majority are benign, there are some clinical and electrocardiographic signs that determine when further investigations may be necessary. Only rarely will palpitations be associated with risk of serious cardiac events.2 This article presents a systematic approach to the patient with palpitations and addresses consideration of the aetiology, history and examination; appropriate diagnostic workup; cardiology/electrophysiology referral and management strategies.
Aetiology
Not all patients with palpitations will have a cardiac or arrhythmic cause. In patients presenting to a university medical centre with palpitations, 41% had an arrhythmic aetiology, 31% had palpitations in the context of psychological disorder such as anxiety, and in 16% no cause was identified.2 In an emergency population, a cardiac cause of palpitations was identified in 34% of patients.3 It is important to caution labelling a patient’s palpitations as being due to anxiety/panic disorder or stress, as 54% of this group will eventually be diagnosed with an arrhythmic cause, and the time delay until arrhythmia diagnosis is 3.3 years.4 Sinus tachycardia may also be a normal response to stress, including episodes of anxiety, and it is important to elucidate cause and effect. Age of the patient may give some indication regarding the arrhythmia mechanism if supraventricular tachycardia is suspected; atrioventricular re-entrant tachycardia (AVRT; Wolf-Parkinson-White syndrome) becomes less likely with increasing age, whereas atrioventricular nodal re-entrant tachycardia (AVNRT), atrial fibrillation and atrial tachycardia become more likely (Figure 1).5
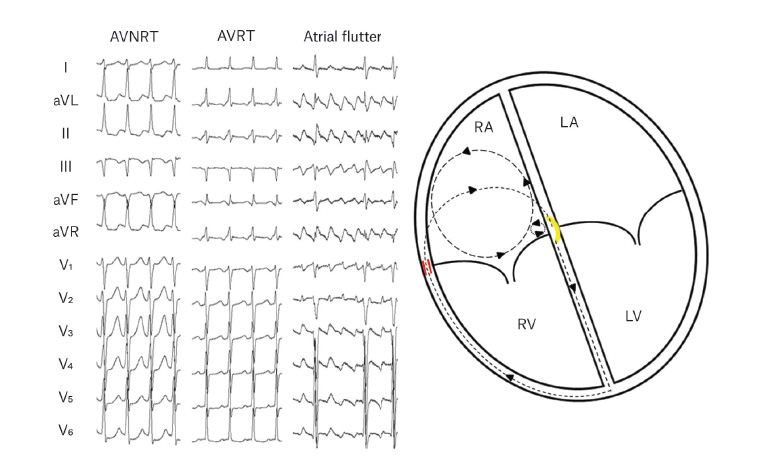
Figure 1. Common types of SVT and representative circuits
The small circuit in dots represents typical AVNRT, short dashes represent (orthodromic) AVRT (via a right free wall pathway represented by the red dashes), and long dashes represent atrial flutter. The yellow arc represents the AV node.
AVNRT, atrioventricular nodal re-entrant tachycardia; AVRT, atrioventricular re-entrant tachycardia; RA, right atrium; LA, left atrium; RV, right ventricle; LV, left ventricle
History and physical examination
History
A thorough history is essential given the overwhelming majority of patients will present in sinus rhythm, between episodes of arrhythmia.1 Palpitations are subjective and have been defined as ‘a disagreeable sensation of pulsation or movement in the chest and/or adjacent areas’;4 it is important to clarify whether the patient’s symptom is palpitations rather than a non-arrhythmic cardiac symptom (eg chest pain, shortness of breath, pre-syncope) or a non-cardiac symptom. Sometimes it is useful to get the patient to tap or clap out the heart rhythm during their typical episode. Once clarified, the history should focus on the nature of the symptoms and circumstances around the time of the palpitations (Box 1).
| Box 1. Palpitations: Key questions in history-taking |
Onset and offset: sudden or gradual
Duration: momentary or sustained (how long?)
Frequency
Triggers (frequently may not be obvious)
Associated symptoms
- Pre-syncope/syncope
- Breathlessness
- Chest pain (possibly ischaemic in nature)
Existing cardiac conditions |
Subjective awareness of a normal heartbeat
One of the causes of palpitations is simply an increased awareness of normal sinus rhythm.6 The patient may describe a forceful beating in the chest or neck that is not particularly fast; they may be able to hear their own heartbeat, particularly at night in bed. Although there may occasionally be secondary causes, in the vast majority of cases this is benign. It may often occur at times of heightened anxiety.
Momentary palpitations: Ectopic beats
Another frequent cause of palpitations is benign ectopic beats, which can be atrial or ventricular.7 Patients describe these as a momentary skipped or missed beat. They are frequently associated with an unusual, momentary sensation in the patient’s throat or chest. Patients usually become aware of ventricular ectopic beats because of a compensatory pause after the ectopic beat, with an associated increase in diastolic filling and supra-normal stroke volume of the post-ectopic sinus beat. Ectopic beats may occur repetitively in patterns (bigeminal, trigeminal, etc) or may be isolated. The frequency of ectopic beats will vary day to day and may be increased under conditions of anxiety, fatigue and inter-current illness. Although doctors frequently recommend patients with ectopic beats to avoid caffeine, there is very little evidence that this is beneficial.8 When asked how long their palpitations last, patients with repetitive ectopy may say that they occur over a period of minutes to many hours. It is important to establish that this is a recurrent, intermittent event rather than continuous rapid palpitations. Previous studies suggest that up to 100 ventricular ectopic beats in a 24-hour period (24-hour Holter monitor) are within normal limits.9 More frequent ectopic beats require further investigation; however, even when a patient has thousands of ectopic beats per 24-hour period, these will most usually be benign and not signify an increased risk of adverse cardiovascular outcomes.
Heart rate devices
It is also common for patients to seek medical attention for ‘palpitations’ when they have recorded what they think may be an abnormal heart rate on a heart rate device such as a fitness tracker or exercise monitor worn around the chest. Patients may be concerned that their resting heart rate is higher than a friend’s or relative’s and wonder whether this signifies a problem. It is important to be able to reassure patients that a wide range of resting heart rates can be within the normal spectrum. These different devices are also prone to error, particularly during exercise, and can erroneously give very high or very low readings.10 The key clue as to whether the heart rate recorded indicates a genuine health problem is the presence of associated symptoms.
Sustained palpitations
Sustained rapid palpitations of gradual onset and offset over minutes or longer periods of time may represent sinus tachycardia. This is also usually benign, particularly at times of anxiety or stress. Less often, sinus tachycardia may signify an underlying disorder such as thyrotoxicosis or anaemia.
Sustained rapid palpitations of sudden onset may be regular or irregular. Patients describe a sudden onset of rapid palpitations that may last from minutes to hours continuously. In the case of atrial fibrillation, this may continue for days or be continuous until treated.
Rapid regular palpitations
In the vast majority of patients, presenting with sudden-onset regular sustained rapid palpitations will signify episodes of supraventricular tachycardia (SVT); in contrast, patients with sinus tachycardia may have a more gradual onset.11 SVT may classically be induced by sudden movements, particularly bending. Many younger patients, including athletes, may describe a sudden onset of excessive heart rate during exertion that may interfere with their ability to compete. However, many patients find no particular trigger, and events can occur at rest. While SVT may cause sudden light-headedness at onset, syncope is unusual. Patients may also complain of chest discomfort or breathlessness during the event.
Patients with sustained palpitations and significant associated symptoms (eg pre-syncope, breathlessness or chest pain) require early referral for evaluation. Patients presenting with syncope or ongoing chest pain should be transferred to an emergency department by ambulance.
Young patients with rapid palpitations, particularly young women, may be misdiagnosed as having panic attacks.Anxiety and distress may be a normal response to an episode of SVT, and the history will clarify whether the SVT or anxiety occurred first.
Patients with SVT can frequently (but not universally) terminate an event with vagal manoeuvres. These include the Valsalva technique or cold stimulus to the face.
Does ventricular tachycardia present as recurrent palpitations?
Patients with ventricular tachycardia infrequently present with palpitations as an isolated presenting symptom. The exception to this may be the relatively uncommon idiopathic ventricular tachycardia, particularly when it is recurrent and non-sustained. In most cases, ventricular tachycardia occurs in the context of underlying structural heart disease (most commonly prior myocardial infarction), and patients present with features of haemodynamic compromise. This may include syncope, diaphoresis, chest pain and breathlessness. Such patients would usually be transferred directly to an emergency department when sustained events occur. As structural heart disease may cause palpitations (and vice versa), it is important to assess cardiac function in patients presenting with palpitations, as abnormalities can significantly affect management and prognosis.
Rapid irregular palpitations: Atrial fibrillation
Patients with paroxysmal or persistent atrial fibrillation may present with sustained palpitations. These are usually described as heartbeats that are very irregular or ‘all over the place’. Patients frequently have associated exertional breathlessness. Syncope due to a rapid ventricular rate in atrial fibrillation is unusual. When patients with paroxysmal atrial fibrillation have syncope, this is frequently due to a significant sinus pause at the time of spontaneous reversion (ie tachycardia-bradycardia syndrome). While chest pain during atrial fibrillation may be solely secondary to a rapid ventricular response rate, if the pain is ischaemic in nature it may reflect underlying coronary artery disease. Polyuria may be associated with paroxysmal atrial fibrillation because of the associated release of atrial natriuretic peptide.12 Atrial fibrillation onset during the night may suggest a vagal mechanism or be a sign of associated sleep-disordered breathing (eg obstructive sleep apnoea). An understanding of the frequency and duration of palpitations over the patient’s life is required, as the symptomatic burden will often define the management strategy (eg conservative management versus medications or electrophysiology study).
The history should include review of background medical issues that may predispose to arrhythmia (eg cardiovascular disease, thyroid illness), psychiatric history, medication history and illicit substances that may contribute to arrhythmia (eg stimulant, weight loss medication). Alcohol history is important given the association of alcohol consumption with the risk of atrial fibrillation.13 Although some patients describe palpitations associated with caffeine intake, a recent study identified no increased risk of any arrhythmia with caffeine intake, even after adjustment for confounders.8 An exercise history could be helpful given that extreme endurance exercise can be associated with the development of cardiomyopathy and cardiac arrhythmia such as atrial fibrillation.14 Family history should be explored, particularly regarding genetic arrhythmia syndromes and history of sudden cardiac death.
A systematic review identified only six factors from the history that significantly correlated with arrhythmia: age of >60 years, regular palpitations, palpitations affected by sleep, regular pounding sensation in neck (atrial contraction against a closed tricuspid valve as in atrioventricular nodal re-entry tachycardia), visible neck pulsations, and vasovagal symptoms (pallor or diaphoresis).12
Examination
Examination will also usually be performed in between episodes of arrhythmia, and it should address any cardiac or systemic illness that might be implicated in the development of arrhythmia including weight (obesity may contribute to atrial fibrillation), resting heart rate, hypertension, signs of heart failure, cardiac murmurs (valvular heart disease), thyroid examination and signs of anaemia. Fluid status and postural blood pressure/heart rate should also be measured, given the association of hypovolaemia with sinus tachycardia and the possibility of autonomic dysfunction when there is an inappropriate sinus tachycardia with postural change. In a systematic review, the only clinical sign that significantly correlated with arrhythmia was abnormal resting heart rate (<60 beats per minute or >100 beats per minute).12
Diagnostic work-up
The gold standard diagnostic technique for a patient with palpitations is to be monitored using a 12-lead electrocardiogram (ECG) at the time of symptoms. However, due to the transitory nature of arrhythmia, this method tends to be the exception rather than the rule. All patients presenting between symptoms should have a 12-lead ECG, because the sinus rhythm ECG can sometimes infer an arrhythmic mechanism (Table 1). Ambulatory electrocardiographic monitoring (eg Holter monitor, external loop recorder, implantable loop recorder, hand-held ECG) can be performed with the goal of correlating a transitory symptom with arrhythmia, and the choice of monitoring should be guided by the yield of the investigation (Table 2). The critical component of interpreting the ambulatory ECG is the rhythm at time of symptoms, and it should ideally also document the arrhythmia onset and/or offset. New technologies such as hand-held ECG (iECG) devices (eg AliveCor Kardia, Semacare Remon) can be considered for the identification of arrhythmia, though these are limited by the cost for the patient to purchase, the time taken to activate the device before arrhythmia termination, and the large amount of data that may be created with no Medicare Benefits Schedule rebate for analysis.
| Table 1. Sinus rhythm ECG markers of arrhythmia1 |
| Electrocardiographic sign |
Implication/consideration |
| Pre-excitation/delta wave |
WPW – AVRT |
| Left atrial enlargement, frequent PACs, sinus bradycardia |
Atrial fibrillation |
| Left ventricular hypertrophy |
Atrial fibrillation, ventricular tachycardia |
| Frequent PVCs |
Ventricular tachycardia |
| Q waves |
Ischaemic heart disease – atrial fibrillation, ventricular tachycardia |
| Widespread T wave inversion across precordial leads, LVH, Q waves and ST-segment changes |
Hypertrophic cardiomyopathy – risk of atrial fibrillation, ventricular tachycardia |
| Long or short QT interval, Brugada pattern, early repolarisation pattern |
Genetic arrhythmia syndromes – risk of sudden cardiac death |
| Inverted T waves or Epsilon waves across right precordial leads (V1–V3)* |
ARVC – risk of sudden cardiac death |
ARVC arrhythmogenic right ventricular cardiomyopathy; AVRT, atrio-ventricular reciprocating tachycardia; ECG, electrogardiogram; LVH, left ventricular hypertrophy; PACs, premature atrial contractions; PVCs, premature ventricular contractions; WPW, Wolff–Parkinson–White
*In patients without right bundle branch block |
| Table 2. Ambulatory ECG monitoring: Choice of investigation |
| Investigation |
Investigation of choice: symptom frequency |
Advantages |
Disadvantages |
| 12-lead ECG |
– |
Readily available
Inexpensive |
Rarely performed during arrhythmia |
| 24–48 hour Holter monitor |
Daily to every second day |
Usually available
Does not require activation: asymptomatic arrhythmia can be detected |
Low yield other than for daily arrhythmias |
Loop/event recorder
(range of 1–4 weeks) |
Weekly–monthly |
Increased yield and cost effectiveness (versus Holter |
Most units only record ECG if patient triggered; not useful for asymptomatic arrhythmia or syncope
Generally only one-week recorders available
Patient discomfort for longer-term monitoring |
| Loop/event recorder for one week |
| Implantable loop recorder |
Months to year/s |
High yield
Long-term monitoring approximately three years
Automatic bradycardia/ tachycardia storage plus patient-triggered episodes |
Cost
Not available in all centres
Currently only approved for diagnosis of syncope or cryptogenic stroke |
| Handheld ECG |
Months to year |
High yield
Permanently available to patient |
Cost to patient
Time for activation of device before arrhythmia termination
Potential large volume of data to interpret, no Medicare rebate
Data ownership with some systems, sometimes requiring subscription |
| ECG, electrocardiography |
In patients with symptoms, risk factors or concern of cardiovascular disease, an echocardiogram should be performed (Figure 2). Where symptoms occur on exertion, an exercise stress test can be considered to both induce and document the arrhythmia, though can often be performed following specialist referral. In rare cases, cardiac magnetic resonance imaging may be considered, again usually following specialist referral.
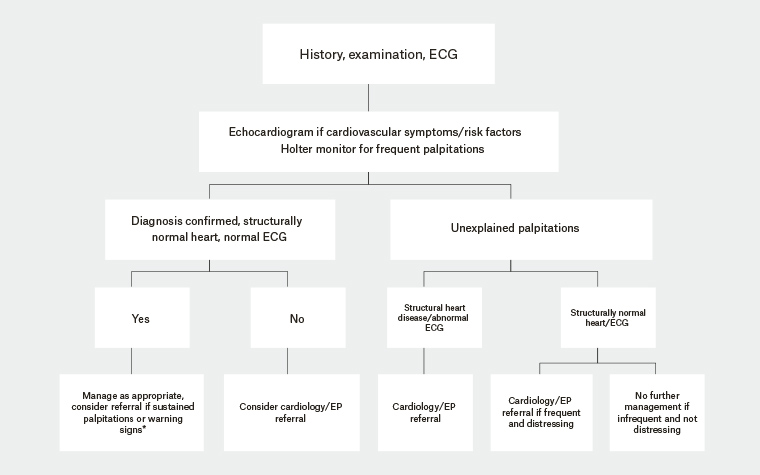
Figure 2. Approach to the patient with palpitations1
ECG, electrocardiogram; EP, electrophysiology
*Refer to Box 2
The initial diagnostic work-up will often be normal; however, if clinical suspicion remains high (such as with a classic history of SVT), specialist referral should be considered for electrophysiology study with or without ablation or implantable loop recorder (ILR). The advantages of electrophysiology studies include identifying the arrhythmia mechanism, potentially curing the arrhythmia during the same procedure, avoiding chronic medication to suppress arrhythmia, and avoiding the delay required to document arrhythmia (eg on serial ambulatory ECG monitoring or ILR); this is especially pertinent if palpitations are associated with syncope or if there is structural heart disease. The risks of performing electrophysiology study include the invasive nature of the procedure (including vascular access complication) and the rare risk of damage to the AV node during ablation. An implantable loop recorder can be considered for patients with sporadic palpitations (<1 per month), often when there is associated syncope.
Referral
Specialist referral should be considered when there may be a substrate for significant arrhythmia, particularly atrial fibrillation and ventricular arrhythmia, given the adverse prognostic implications associated with these arrhythmia. This may be suggested by:
- a history of structural heart disease; abnormal ECG or echocardiogram
- palpitations associated with syncope, presyncope or chest pain
- family history of sudden cardiac death
- high clinical suspicion in a patient with sustained palpitations.
Specialist referral will often be required after the initial diagnostic work-up has been completed for consideration of, and access to, longer-term monitoring or electrophysiology study with or without ablation.
Management
The management of palpitations will depend on the arrhythmia mechanism and implicated prognosis. Many patients with a subjective awareness of their own heartbeat or infrequent palpitations consistent with ectopic beats can be treated with reassurance and support.
Box 2 includes a list of which patients should be considered for referral. Patients with certain occupations (eg pilots, commercial truck drivers) will require specialist referral for consideration of occupational implication, diagnostic and treatment strategies. Patients with suspected or documented SVT should be educated regarding the Valsalva manoeuvre, which can often terminate arrhythmia.
| Box 2. Which patients to refer or ‘When to worry’ |
Patients with frequent or persistent palpitations
Sustained rapid palpitations
Significant associated symptoms:
- Pre-syncope/syncope (consider situational context)
- Breathlessness
- Chest pain
Family history of recurrent syncope or of sudden death
Significant resting 12-lead electrocardiography or echocardiographic abnormalities
- Wolff–Parkinson–White syndrome (pre-excitation including short PR interval and delta wave)
- Signs of structural or electrical abnormalities:
- T wave abnormalities
- Prior myocardial infarction (Q waves)
- Long or short QT interval, Brugada pattern, early repolarisation pattern
|
Conclusion
Palpitations are common and, while usually benign, may rarely be associated with adverse prognosis. A structured approach will often identify the arrhythmia; however, specialist referral will be sometimes required for both diagnosis and treatment.